Feature | Serving A Unique Population: Caring for the Cardio-Rheumatology Patient

While modifiable risk factors for cardiovascular disease are well known, several additional factors have been identified that increase cardiovascular risk.
One important, and often overlooked, risk factor is systemic autoimmune disease.
Rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis and psoriatic arthritis (PsA) are examples of chronic inflammatory rheumatologic diseases that are associated with an increased risk of cardiovascular events (Figure 1).
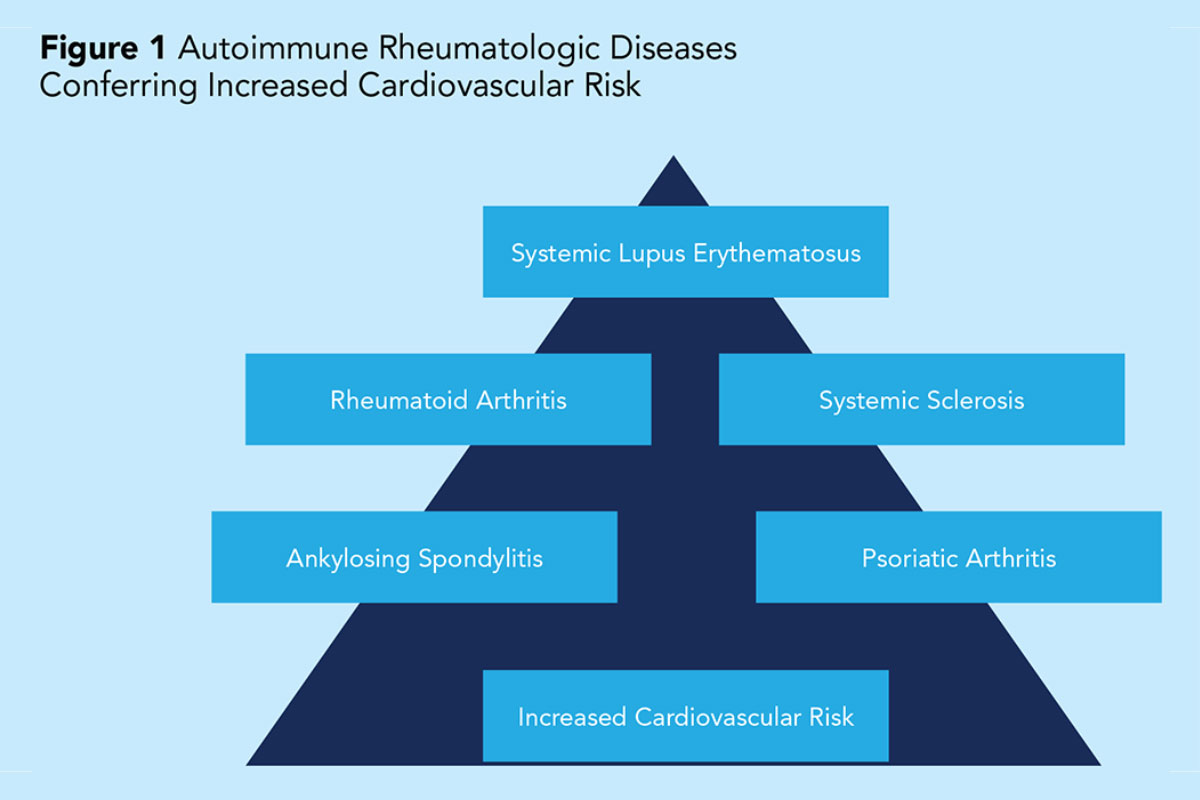
While the association between systemic autoimmune diseases and cardiovascular disease has been well documented in the literature, the mechanism is not fully understood. However, there is a plethora of supporting evidence that RA, SLE and PsA confer an increased risk of cardiovascular disease not accounted for solely by the prevalence of modifiable risk factors in these patients.
The leading hypothesis suggests that a combination of factors play a role in the increased cardiovascular risk, including a higher prevalence of traditional cardiovascular risk factors, chronic systemic inflammation, proinflammatory HDL-C, disease-specific risk factors (immune-complex factors, circulating inflammatory cytokines, and antiphospholipid antibodies) and effects of anti-inflammatory drugs.
An estimated 1.3 million Americans are affected by RA.1 Patients with RA have a 2-fold greater risk of developing heart failure and a 1.5-2-fold increased risk of coronary artery disease (CAD) compared with the general population.2 Cardiovascular disease is the leading cause of morbidity and mortality in patients with SLE.
There is a 50% increased risk of cardiovascular mortality among patients with RA compared with non-RA patients. In fact, cardiovascular morbidity and mortality in RA patients are similar to that seen in patients with diabetes mellitus.3
Premature atherosclerosis is a contributing factor for the increased prevalence of coronary heart disease in patients with SLE and RA. Additionally, the formation of a psoriatic plaque shares a common pathway with the atherosclerotic process.4 This may partly explain the increased cardiovascular disease rates in patients with PsA. Proinflammatory HDL-C is also found in nearly one-half of SLE patients, contributing to the development of atherosclerosis.5
Gaps in CV Risk Assessment and Symptom Recognition

Our current risk assessment tools do not accurately estimate cardiovascular risk in patients with systemic autoimmune diseases. The ACC/American Heart Association Cardiovascular Risk Calculator, Reynolds Risk Score, and the Framingham Risk Score have been shown to underestimate cardiovascular risk in patients with systemic autoimmune conditions.6
Both RA and SLE occur at higher rates in women than men. Although chest pain remains the most common presenting symptom for women with CAD, patients with RA and SLE often have atypical symptoms. RA and SLE patients presenting with CAD are often young women in whom providers have a low suspicion for coronary heart disease.
This observation, combined with an atypical presentation of CAD, can result in under-recognition of angina, resulting in a delay in appropriate and timely evaluation of symptomatic patients. In fact, RA patients are twice as likely to have had a silent myocardial infarction compared with non-RA patients.7
Not only are providers at risk for overlooking these symptoms, but so are our patients. A 2014 survey by the Women's Heart Alliance demonstrated that 45% of women were unaware that heart disease was the leading cause of death among women.8 Only 19% of women were aware of the association between autoimmune diseases and heart disease.8
Studies have shown that awareness of cardiovascular disease risk correlated with likelihood of initiating risk factor prevention and treatment among patients.4,9 Therefore, it is imperative that we increase awareness among patients with chronic autoimmune diseases, and their providers, about the symptom presentation and increased cardiovascular risk in this group.
Missed Opportunities For Prevention and Intervention

Hypertension and hyperlipidemia are often underdiagnosed and undertreated in patients with RA.2,10 Studies have also shown a higher prevalence of hypertension in patients with psoriasis.11,12 Sabio, et al., found a higher incidence of hypertension in women with SLE compared with controls and this disparity was more pronounced in younger patients (40% vs. 11%; p<0.001) compared with older patients (74% vs. 47%; p=0.0010).13
Unfortunately, even among those diagnosed with hypertension and hyperlipidemia, a disproportionate number are not adequately treated. One study demonstrated that among RA patients with hypertension and at increased cardiovascular risk, only 23% were on antihypertensives. Among those treated for hypertension, 50% had a systolic blood pressure >140 mm Hg.14
Another study showed that among RA patients who were candidates for lipid-lowering therapy, 40% of them were not on a statin.15 These examples represent missed opportunities to modify CV risk in patients prior to development of clinical heart disease. Given the increased risk of cardiovascular disease in patients with systemic autoimmune diseases, early identification and intervention of modifiable risk factors are of critical importance.
The use of noninvasive diagnostic tests to screen for cardiovascular disease is helpful in the assessment of patients with chronic autoimmune diseases. Identification of subclinical atherosclerosis on carotid artery ultrasound or cardiac computed tomography can further guide recommendations for aggressive management of cardiovascular risk factors and statins for primary prevention of cardiovascular disease.
Recommendations For Collaborative Care

One of the challenges in the care of patients with systemic inflammatory diseases is that their medical conditions are often managed by multiple providers. At times, it may be unclear who is responsible for managing hypertension if a patient is not at goal. Should the primary care provider, rheumatologist, nephrologist or endocrinologist take the lead in ensuring the blood pressure or cholesterol are adequately treated?
Given that these patients are at increased cardiovascular risk, I recommend a preventive cardiologist be included as a member of the patient's care team. The cardiologist can emphasize cardiovascular disease risk, and monitor drug-related cardiovascular side effects.
Patients with chronic autoimmune diseases are less likely to be physically active compared with those without autoimmune diseases. Periods of increased disease activity result in joint pain and fatigue, discouraging patients from engaging in exercise. Suffering with a chronic autoimmune disease can contribute to mood disorders, such as depression, making it even more difficult to find the motivation for regular exercise.
However, it is important that we reinforce to patients the benefits of exercise on cardiovascular risk and mood stability. I often recommend water aerobics or low-impact aerobic exercise such as walking for my cardio-rheumatology patients.

I encourage them to divide their exercise sessions into more manageable, smaller time periods (10-minute blocks) in order to accomplish their goal. I empathize with their inability to exercise when during a flare, but recommend they resume their exercise program once they have clinically improved. Regular exercise has been shown to improve cardiorespiratory fitness and cardiovascular risk factors in RA patients without worsening disease activity.16
Consultation with an exercise physiologist or clinical dietitian can provide patients with exercise and dietary counseling complementary to those discussed with a preventive cardiologist. Consideration of referral to a psychologist or psychiatrist for anxiety and depression cannot be overstated given the physical, psychological and debilitating complications of chronic autoimmune diseases.
As the cardiology field expands to include newer subspecialties, we must not lose sight of the importance of cardiovascular disease prevention. While we are accustomed to screening for heart disease among patients with a family history of heart disease or those with traditional cardiovascular disease risk factors, there is another population often overlooked and undertreated.
Cardiology-rheumatology patients are at increased risk for cardiovascular disease and warrant the care of a multidisciplinary team that includes a preventive cardiologist to focus on cardiovascular risk factor screening, aggressive risk factor modification, evaluation and treatment of symptomatic patients and education of patients and providers regarding their increased cardiovascular risk.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Atherosclerotic Disease (CAD/PAD), Nonstatins, Novel Agents, Statins, Exercise
Keywords: ACC Publications, Cardiology Magazine, Coronary Artery Disease, Risk Factors, Cardiovascular Diseases, Arthritis, Psoriatic, American Heart Association, Cause of Death, Atherosclerosis, Cytokines, Antigen-Antibody Complex, Prevalence, Arthritis, Rheumatoid, Angina Pectoris, Risk Assessment, Lupus Erythematosus, Systemic, Antihypertensive Agents, Blood Pressure, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Antibodies, Antiphospholipid, Hyperlipidemias, Walking, Motivation, Incidence, Rheumatology
< Back to Listings