Cover Story | Team Up: Patient-Centered Geriatric Cardiology

The patient is a 75-year-old African American woman who is thin and frail. She has a history of coronary artery disease with two NSTEMIs in the past three years. Catheterization showed a 90% blockage in the left anterior descending artery.
She also has some mitral valve disease, diabetes, chronic kidney disease, hypertension, hyperlipidemia, peripheral artery disease, atrial fibrillation (AFib), osteoarthritis, hypothyroidism, and heart failure with reduced ejection fraction (left ventricular ejection fraction [LVEF] of 20-30%).
She is taking at least 13 prescription medications. She comes to your office to discuss the possibility of coronary artery bypass surgery (CABG).
This is a real patient. We'll call her Linda. When Larry A. Allen, MD, MHS, FACC, professor of medicine at the University of Colorado, Anschutz, presented this case during ACC's Heart House Roundtable on navigating treatment decisions for patients with atherosclerotic cardiovascular disease and multiple comorbidities, the clinician audience was quiet.
Then one spoke up: "I'm glad she's your patient."
In reality, Linda is everyone's patient.
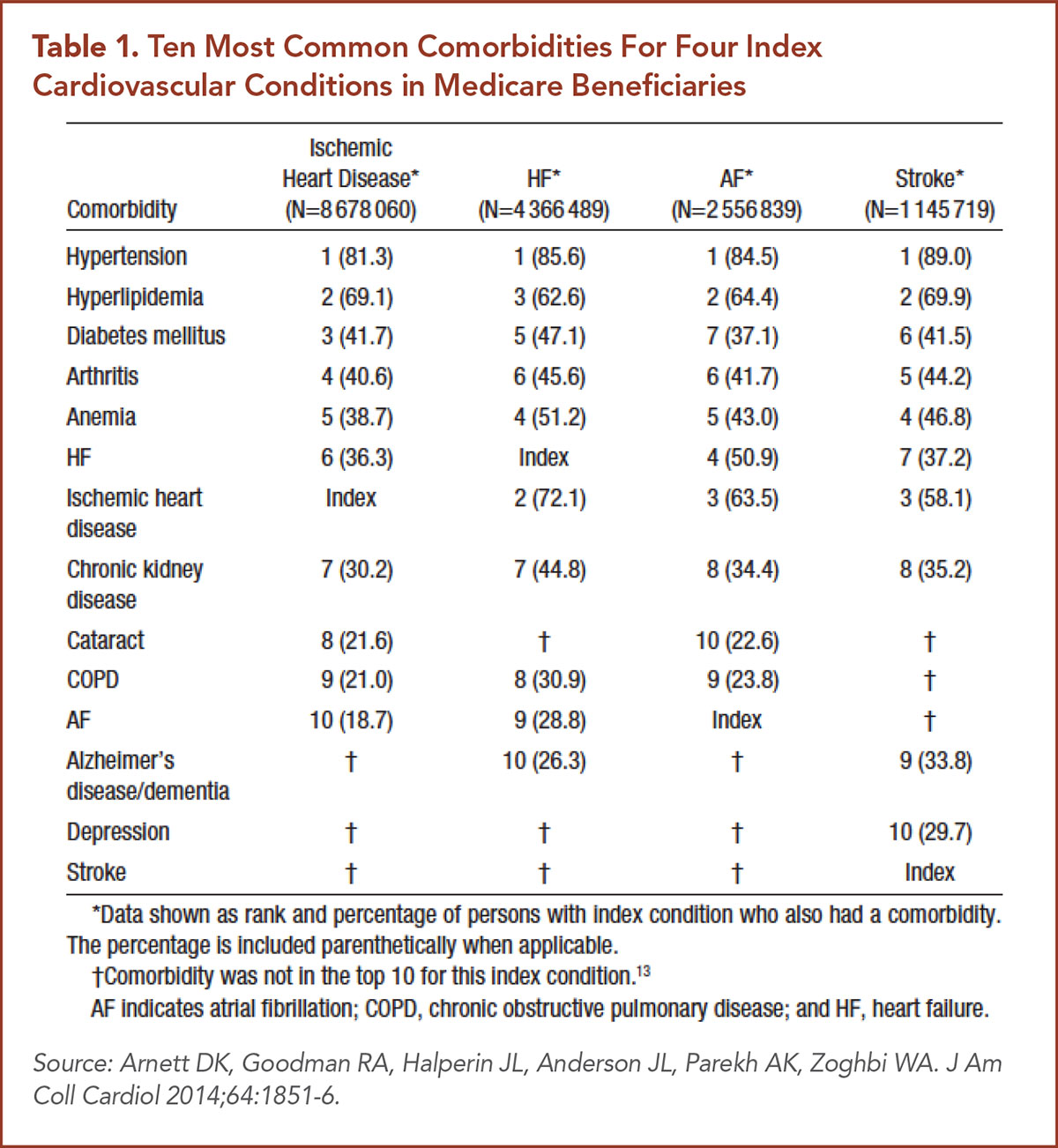
More than 80% of individuals ages 65 and older with ischemic heart disease, heart failure, AFib, and/or stroke also suffer from hypertension; more than a third have diabetes (Table 1).
Other common comorbidities include arthritis, anemia, and chronic kidney disease. Overall, 68% of Medicare beneficiaries have two or more chronic conditions, and 14% have six or more.1
And that doesn't count "hidden" comorbidities such as frailty and cognitive dysfunction.
"I have a lot of patients like Linda," Allen says. "To some extent, this is a product of success through improved medical technology, in that we're able to treat, but not cure, many diseases, so patients live with them longer," he notes.

"They're older, struggling with not being able to do as much as they're used to, and trying to manage complex diseases like diabetes and heart failure that require a lot of day-to-day management. If they're feeling ill or have dementia that just complicates things."
The combination of obesity, diabetes, and cardiovascular disease in particular "is a real challenge because each individual problem is complex in its management and when you put them together it can be overwhelming for patients as well as clinicians," says Allen.
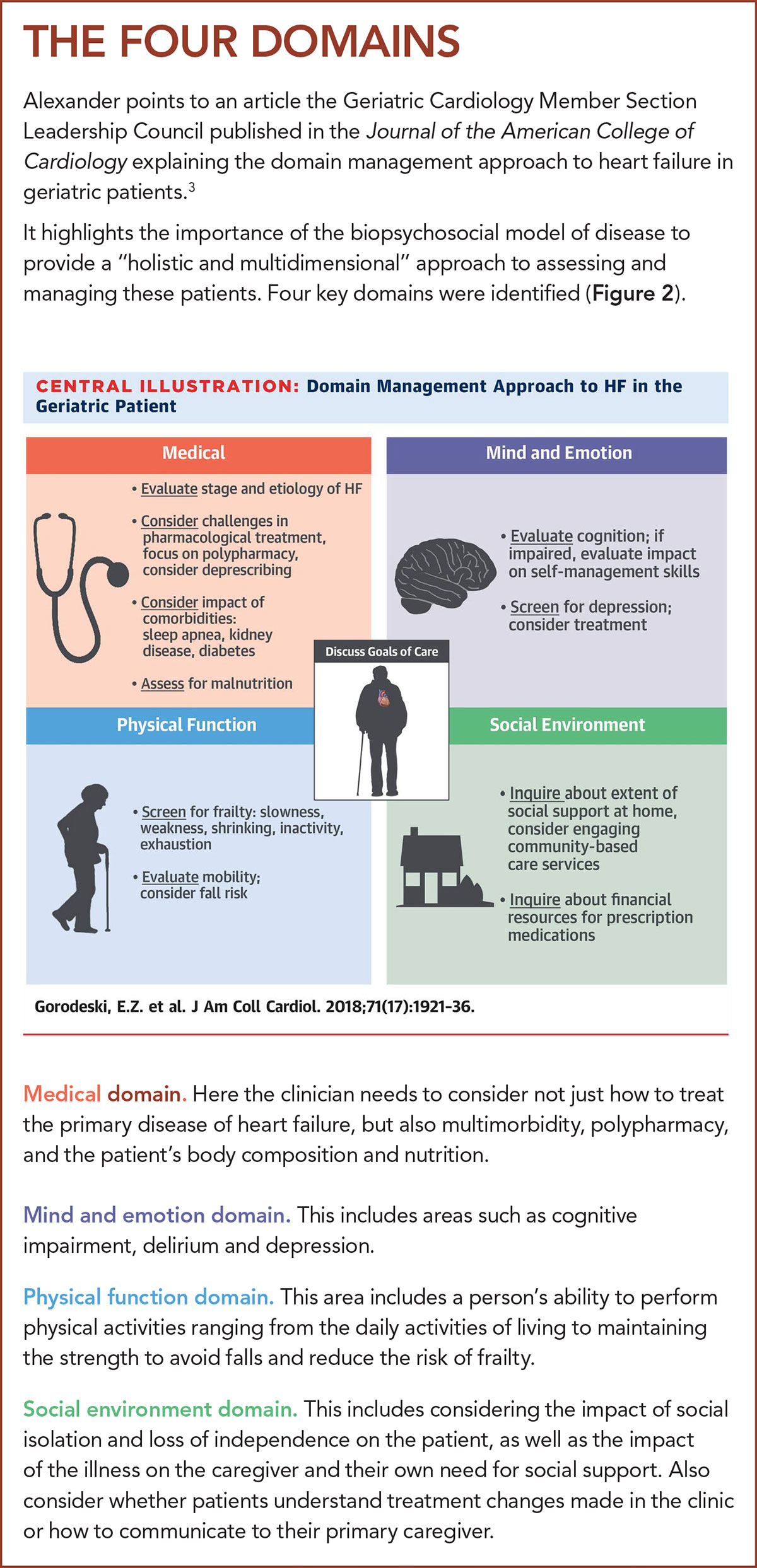
"One main takeaway from this concept of multimorbidity is that even though we, as cardiovascular specialists, are very good at focusing on our particular organ, the reality is that our older patients have many comorbidities that affect their cardiovascular disease," says James N. Kirkpatrick, MD, FACC, professor of medicine at the University of Washington Medical Center in Seattle, and chair of ACC's Geriatric Cardiology Member Section Leadership Council.
"It's important for us to realize the effect that has on quality of life."
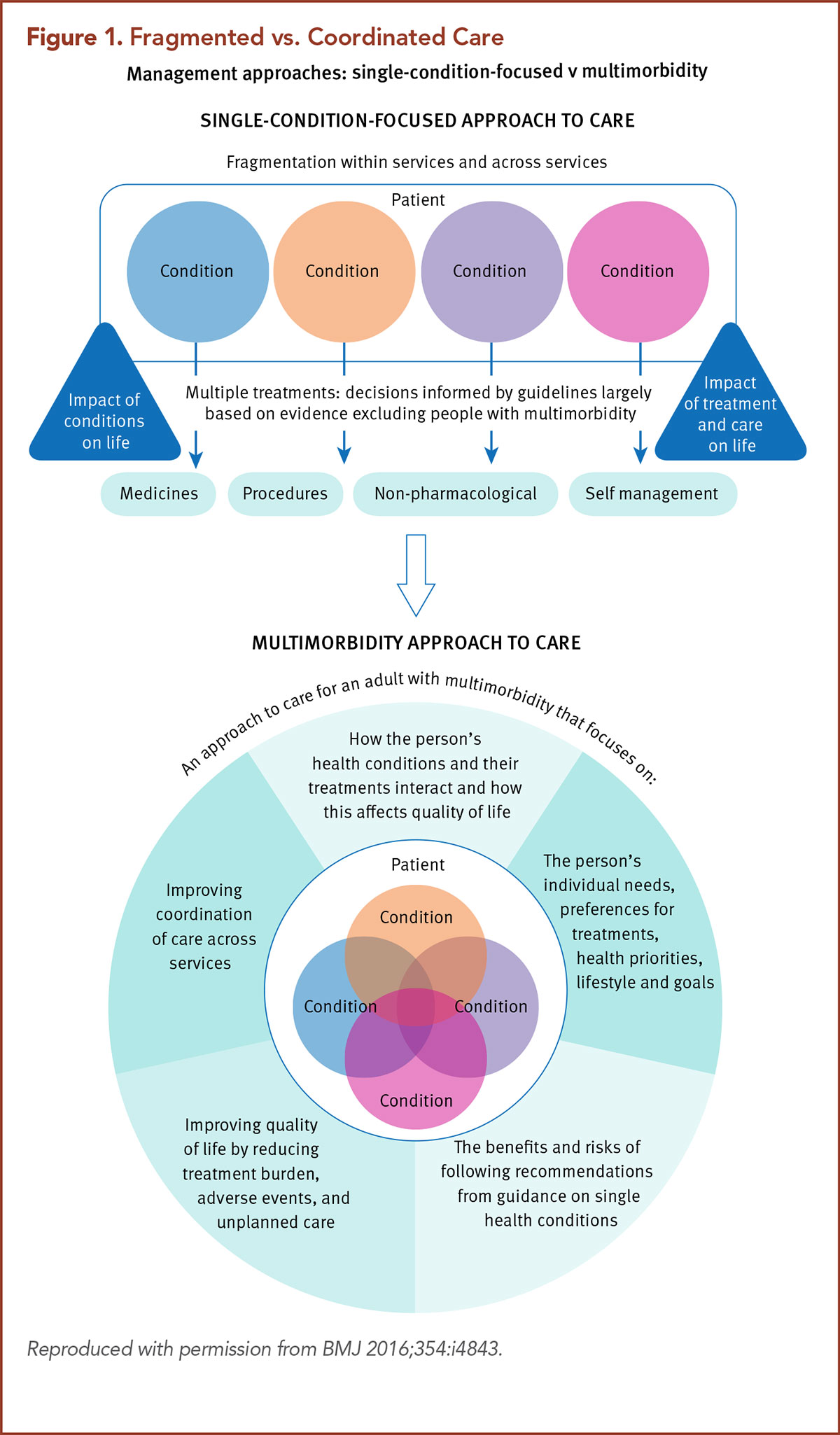
Indeed, during the Heart House Roundtable speakers stressed the need to consider patient preferences and priorities in developing a framework for care, including the impact of treatment on quality of life, as well as its expense and other personal objectives (Figure 1).
Rather than the traditional, paternalistic approach in which the clinician unilaterally determines the treatment plan, a shared decision-making approach takes into account the patient's values and preferences and is particularly important in the older population with multiple morbidities.
"The patient is the expert on the patient," says Kirkpatrick. "Starting with the goals of care allows us to take the cardiovascular diagnosis and prognosis and merge those with things like the patient preferences, values and goals. Then it becomes a discussion between two experts, the patient and the physician, to try to come up with an approach that matches what we do with what's important and what's achievable and reasonable to do."
What it doesn't mean is expecting the patient to be the medical expert and choose the treatment from a shopping list of options, he says.
"You need to put the treatment of the heart in context with the rest of the person, not in isolation," says Karen P. Alexander, MD, FACC, professor of medicine at Duke University in Durham, NC, and immediate past chair of the Geriatric Cardiology Member Section Leadership Council.
"Also, we need to remember the goal is to help patients either feel better, avoid future adverse health events, or live healthier for longer – and some things that we do sometimes don't accomplish these goals."

"If we demonstrate that what the patient brings to the table is important in the decision-making process, then they are more likely to open up," says Kirkpatrick.
"This has huge implications, not just for people who want to do the right thing and follow our recommendations, but even the people who are little bit hesitant about trusting us."
And when patients trust their health care providers, he says, treatment adherence can improve. Sometimes, older patients with many comorbidities or their families may insist on therapies that clinicians believe are inappropriate.
"Some of the controversy over requests for care that we think might not be appropriate can be resolved through very open and honest communication," Kirkpatrick says. "It's important to unpack and understand what might be driving these discussions."
For instance, he described a hospitalized patient in late-stage heart failure who was resisting comfort care. "He was clearly dying and there were no other options," Kirkpatrick says. But the patient and his family continued to insist on the "full court press" of all treatments.
"Something wasn't quite right, and the clinicians were getting frustrated," Kirkpatrick recalls. But more conversations revealed that the man's large family, who had been visiting him in the hospital and bringing meals, felt the nurses resented them and didn't respect their cultural habits.
"As soon as that came out, the staff apologized and assured them that they wanted to provide the right kind of care." That resulted in an immediate resolution and the patient decided to go with the recommendation for palliative care.
Setting Goals
Goal setting is not always as straightforward as it might seem. "We talk about the importance of patient goals, values and preferences," says Allen, "but patients themselves may struggle with defining their core values and what they want."
Often, patients say they want to live as long as possible, but at the same time they don't want a burdensome treatment.
"Helping them choose what to do is part of the art of medicine," he says. "It's having those tough discussions about tradeoffs."
Take, for instance, the patient or family members who demand that "everything be done," even in late-stage heart failure. When that happens, says Kirkpatrick, "we need to unpack that and see what's underneath." If their goal is longevity, "you need to find out what they're willing to do to reach that goal."
In addition, he says, "You need to highlight that prolonging life and quality of life are not necessarily both achievable."
It also requires taking the long view rather than focusing just on short-term biometrics, and understanding that patient priorities may change over time. For instance, a 70-year-old with heart failure may prioritize gardening as a priority, while in 10 years the priority might be to attend her granddaughter's wedding.
It's also important to recognize that patients and clinicians are often driven by different priorities. While the patient's priorities may be symptom management, concerns and frustrations, the provider's priorities may be driven by disease risk, quality measures and prior visit plans. Yet even in a time-limited visit, these goals can be aligned through a focused discussion.2
Team-based Care

Caring for older patients with multiple morbidities requires interfacing with other physicians treating that patient and understanding their treatment plans, says Kirkpatrick. This can be done by communicating through the electronic medical record, he notes, but this may not be sufficient, and a direct call or patient-care conference may be necessary.
Indeed, Allen highlights the problem that even within the cardiovascular field, "specialty" care has been fragmented into health care silos that challenge the clinician's ability to communicate between providers and create a coordinated plan.
"Many of my patients see an electrophysiologist and a lipid specialist. There is overlap with diabetes and heart failure. It all adds to the complexity. So how do you take a step back and look at it from the patient perspective and put it all together so you're getting a global view of things?"
Allen highlights three key steps clinicians should take:
- Always consider the patient perspective and the totality of what the patient is experiencing.
- Facilitate communication between specialists through the electronic health record and other technologies.
- Consider where the patient is in the course of their lifetime. "As patients get older and have a shorter life expectancy with more chronic conditions you have to take a step back and try to simplify the way we treat those diseases. Trying to treat them all with every therapy becomes untenable." This is where an integrated approach that considers both the patient's medical condition and health outcomes and goals becomes so important.
What's vitally important, Alexander says, is to develop a relationship with the patient and understand that it's not just the specialist but the care team.
"There needs to be a sense of connection with these complex patients so they feel safe reaching out," she adds.

Sometimes the cardiologist may feel intimidating and the patient doesn't want to "bother" them, she notes. A nurse or other team member might be able to connect more quickly or at a different level.
"We need to create more space and time for patients," says Allen.
"We need to recognize that they can be deferential sometimes because they don't have a full grasp of the medical issues. If you empower them to understand the details of the medical decision in front of them, they want to take back that control and say, 'This what I want as patient.'"
And Linda? "We had some tough conversations about her undergoing CABG," says Allen.
"I was worried that her risks of complications were high and that the potential benefit might be less than for the average person. But in talking with her she still very much wanted to optimize her chance to live longer and feel better, so she was willing to be more aggressive and take some risks. Her postoperative course was somewhat initially rocky, as expected. But fortunately, she's currently doing very well."
Conversations Around COVID-19

The pandemic has brought a new wrinkle into the cardiovascular clinic, whether virtually or in person. The specialists interviewed here all talked about their patients' fears of coming to the hospital, even for acute conditions. "There's really a fear that hospitals are 'COVID hotels,'" says Kirkpatrick.
Yet it can be hard to communicate that to patients who too often fall into what Alexander calls "the COVID hole," and ignore potentially serious symptoms. Alexander shares that one of her patients with atrial fibrillation who was scheduled for cardioversion in March, didn't follow up until midsummer – remaining in AFib the entire time. Yet, says Alexander, "She was terrified of coming into the hospital for treatment."
Part of the COVID discussion centers around the fact that people with underlying conditions like heart disease have a higher risk of poor outcomes if they develop the disease, says Kirkpatrick. He uses that as an opportunity to stress the importance of advanced care planning with a living will and durable power of attorney.
All of which gets back to patient preferences. "Combine multiple medical problems in an older person with COVID-19 and it is quite dangerous," says Allen.
"This also raises questions about how to treat high-risk patients with COVID-19 who become very ill and may need mechanical ventilation to stay alive. In such patients, having previously considered goals of medical care is important."
CardioSmart: Supporting the Patient-Physician Dialogue
From infographics to decision aids, ACC's CardioSmart provides the tools to guide the discussion between patients and physicians, helping patients to understand their conditions and reach the best decisions for their goals. Visit the new CardioSmart site at CardioSmart.org to explore and download tools.
Editor's Note: In this article and on the cover, you may notice the photo shows clinicians and patients in a pre-COVID-19 environment. In the current era of COVID-19, the ACC encourages all clinicians and patients to #MaskUp as part of CDC-recommended guidance to stop the spread. Share your photo of you and/or your colleagues in your mask using #CardiologyMag and #MaskUp.
References
- Arnett DK, Goodman RA, Halperin JL, Anderson JL, Parekh AK, Zoghbi WA. AHA/ACC/HHS strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions: from the American Heart Association, American College of Cardiology, and US Department of Health and Human Services. J Am Coll Cardiol 2014;64:1851-6.
- Grant RW, Adams AS, Bayliss EA, Heisler M. Establishing visit priorities for complex patients: A summary of the literature and conceptual model to guide innovative interventions. Healthc (Amst) 2013;1:117-22.
- Gorodeski EZ, Goyal P, Hummel SL, et al. Domain management approach to heart failure in the geriatric patient: Present and future. J Am Coll Cardiol 2018;71:1921-36.
Clinical Topics: Arrhythmias and Clinical EP, COVID-19 Hub, Dyslipidemia, Geriatric Cardiology, Atherosclerotic Disease (CAD/PAD), EP Basic Science, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: ACC Publications, Cardiology Magazine, Atrial Fibrillation, Stroke Volume, Coronary Artery Disease, Goals, Quality of Life, Peripheral Arterial Disease, Myocardial Infarction, Prevalence, Hyperlipidemias, Patient Preference, Medicare, Palliative Care, African Americans, COVID-19, Pandemics, Aged, Living Wills, Electronic Health Records, Life Expectancy, Patient Preference, Electric Countershock, Frustration, Lawyers, Longevity
< Back to Listings