Feature | Acute Decompensated Heart Failure: The Need For The Patient's Perspective
Understanding the perspective of the patient can assist clinicians and patients in creating sustainable, high value, actionable items for self-care of acute decompensated heart failure (ADHF). A study conducted by the ACC suggests patients are willing to perform these items if they remember the instructions.

Knowing Signs and Symptoms
In general, survey respondents expressed confidence in knowing when HF decompensation occurs and when to seek help.
The most frequently (>50%) reported symptoms indicating decompensation included shortness of breath (81%); fatigue and weakness (71%); swelling in legs, ankles and feet (68%); and rapid and irregular heart beat (57%). Most respondents were at home – sitting (26%), in bed (16%), working (13%), going up the stairs (12%), working in the yard (10%) – when they first noticed decompensation symptoms.
A minority said they were "shopping/running errands" or at a "doctor's appointment." For those at the doctor, it could not be determined from the questionnaire if these patients failed to recognize their symptoms earlier or recognized them but waited to discuss symptoms with a clinician.
Nearly 80% of respondents sought help within 12 hours of the onset of decompensation with nearly half seeking help within the first hour. There was greater delay (>12 hours) in seeking treatment by respondents who had no previous HF hospitalization compared with those with prior hospitalization (35% vs. 14%; p<0.001).
Fourteen percent waited longer than two days to seek help. Most patients indicated they were driven by a family member to the hospital (45%), followed by an ambulance (26%) or driving themselves (11%).
Upon recognition of HF decompensation, most respondents said they felt "stressed" (65%), "scared" (60%), "anxious/nervous" (59%) and "fearful" (52%). However, many reported feeling decreased levels of stress, fear and nervousness at discharge.
Self-Care and Medication Adherence
The majority of respondents reported "taking all medications as prescribed," and "taking the right medication" regardless of their HF duration. Patients reported "cutting down on sodium" consistently, at 83% overall.
However, the actual tracking of sodium intake varied over time, starting at 43% (<1 year), increasing to 51% (1-2 years), and decreasing to 39% (>5 years).
Adherence to prescribed diuretics started at 54%, increased with HF duration to a peak of 79% (3-4 years), but dropped off slightly to 77% at HF duration >5 years.
"Watching for worsening HF symptoms" undulated but trended positively with HF duration reaching 77% with HF duration >5 years. Tracking daily weight held steady at 54% regardless of disease duration.
Seeking help for fluid weight gain increased from 49% (<1 year) to 70% (3-4 years); however, this action dropped to 44% at HF duration >5 years.
Correlation analysis on reported self-care actions to HF duration found that "visit physician regularly" positively correlated with HF duration (80% at <1 year to 91% at >5 years; r=0.997; p=0.003). Other self-care actions did not achieve statistical significance in correlation with HF duration.
Some conditional associations of symptom recognition, self-care monitoring and seeking timely medical intervention were identified.
For example, a majority of those (59%) who reported sudden weight gain from fluid retention also tracked daily weight.
Those who tracked daily weight were more likely to seek help with fluid weight gain than those who didn't track (71% vs. 39%; p<0.001).
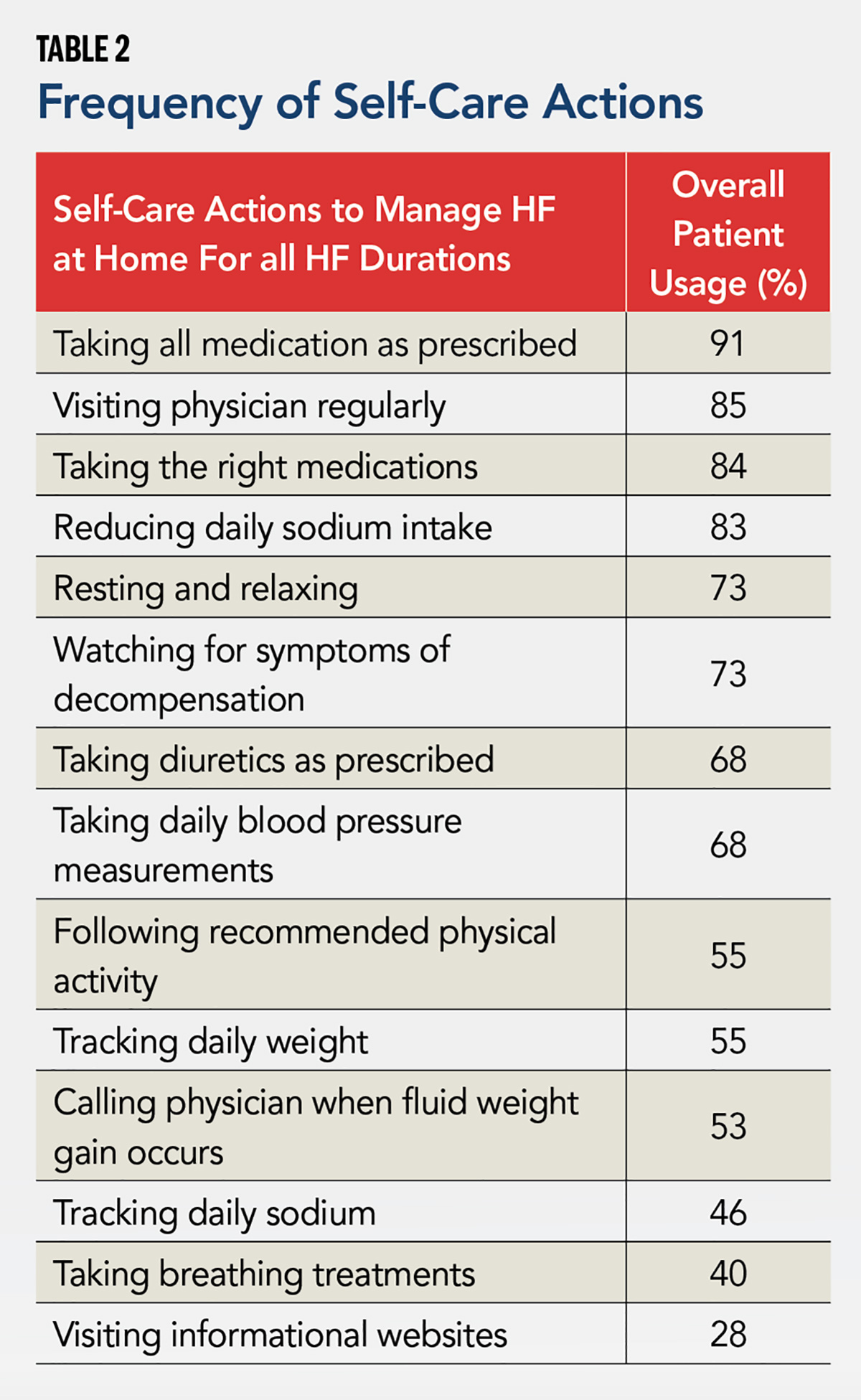
In general, a large scatter existed for remembered instructions and reported self-care actions. Self-care actions that showed moderate correlation with remembered instructions included taking blood pressure daily, tracking sodium daily, taking diuretics as prescribed and tracking daily weight. The remembered instruction of "following up with your doctor within a week of your discharge" correlated with the highest number of reported self-care actions.
In addition to self-care actions (Table 2), the survey also examined use of commonly provided services. Respondents most commonly reported: follow-up phone call (47%); blood pressure monitor that transmits readings (36%); visiting nurse/visiting nurse service (29%); and low-sodium meal service (26%).
Patient use of/participation in a low-sodium meal service, cardiac rehabilitation, a scale that notifies doctor of weight fluctuation and HF clinic monitoring decreased with duration of HF diagnosis. Despite the decreasing use of automated notification scales, patients continued to track their weight. The services queried may not have been uniformly available to all respondents; therefore, reported usage rates may have been affected by availability.
What Do These Findings Mean?

The study adds to the literature on patient experience by reflecting the journey of the HF patient, both before and after hospitalization, by exploring areas that were not in previous smaller self-care studies.
These findings demonstrate and support that:
- Patients are confident in identifying decompensation.
- Patients who experience ≥1 HF admission will seek care promptly with decompensation.
- Women with HF are socio-economically disadvantaged.
- Performance of self-care actions does not improve with duration of HF.
- Patients can perform self-care actions if instructed.
The study results emphasize the necessary components for an effective patient-centered HF program. Not only is recognition of the patient experience crucial, but a program needs to nurture patients' capacity for self-care and self-efficacy. For women, because living alone and lower income can increase mortality, an effective patient-centered program for HF care will need to address these issues.
Sustained training with follow-up coaching can grow the identified potential into significant improvements in self-care. Improvements gained from better self-care may lead to less depression, thereby further increasing effectiveness.
Since patient self-care can provide timely if not immediate intervention, improved self-care may succeed where interventions that rely on technologies and external instructions, which can be delayed by days, have not made significant differences.
Methods and Patient Demographics

The ACC, with funding support from Novartis, conducted a 48-item online survey through three different consumer panels (Research Now, Toluna, Harris Poll). Of the total 14,720 survey respondents across the three panels, 331 met the inclusion criteria consisting of: patient age ≥50 years; persistent HF symptoms; hospitalized for ADHF within four months of the survey. The Chesapeake Bay Institutional Review Board Services conducted the independent review and approved the protocol used for the study.
Of the patients who met the inclusion criteria, 52% were male and 46% were female, while 2% declined to answer. The majority of respondents were Caucasian (82%), followed by Hispanic (10%) and African American (8%). Broken down by age, 58% of respondents were between the ages of 50-59, followed by 60-69 years (26%) and 70-79 years (16%). More than half of respondents (58%) reported an annual income ≤$50,000/year, which fell below the 2014 U.S. median income of $53,657.
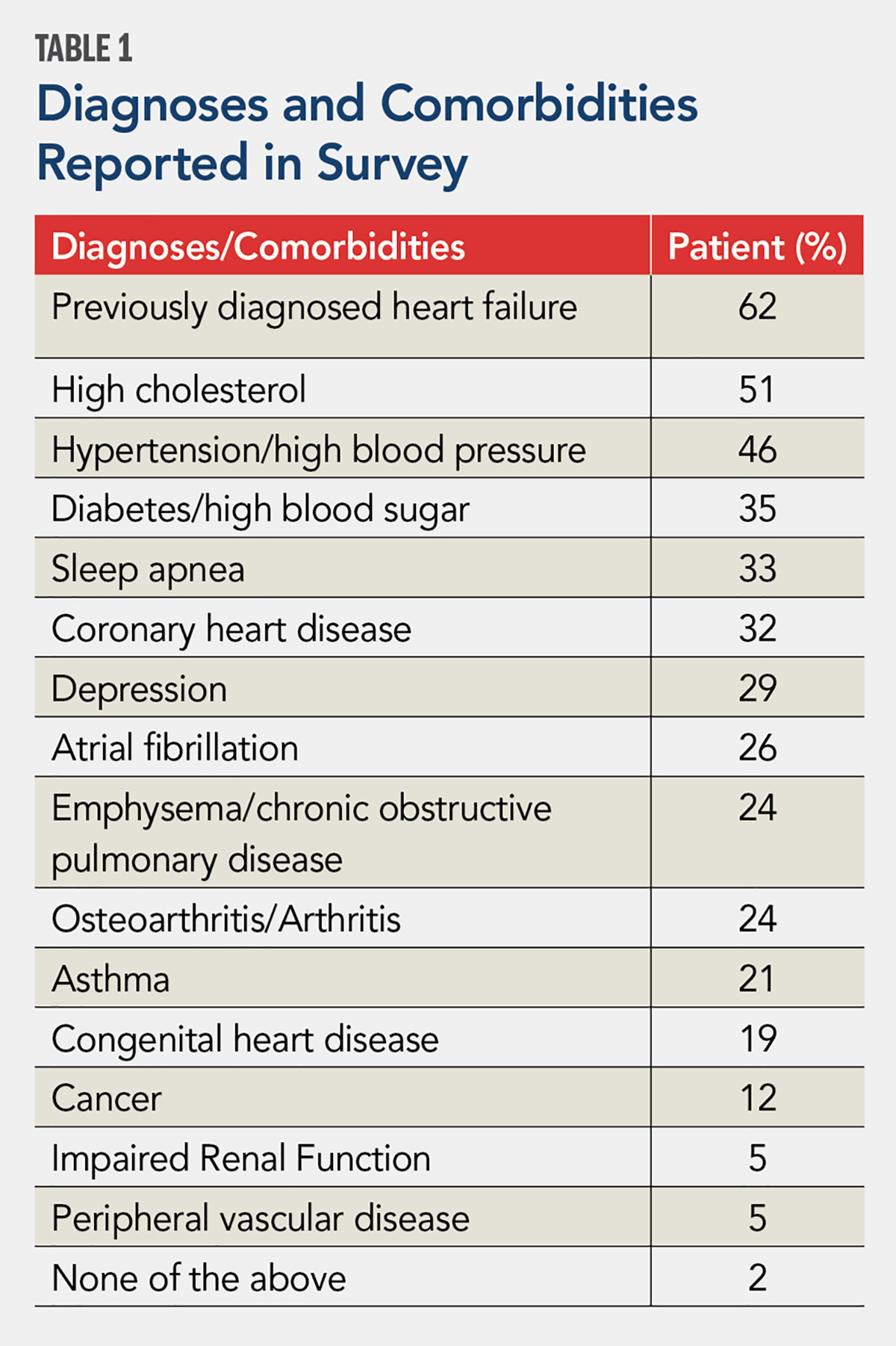
In terms of health, most patients (62%) indicated having been diagnosed with HF prior to the qualifying hospitalization. Frequently occurring diagnosed comorbidities (i.e., >25% of respondents) included high cholesterol (51%), hypertension (46%), diabetes (35%), sleep apnea (33%), coronary artery disease (32%), depression (29%) and atrial fibrillation (26%).
A substantial number of respondents (27%) carried a diagnosis of HF for ≥5 years. HF hospitalization was common, with 17% of respondents reporting five or more previous hospitalizations. Their diagnoses and comorbidities are detailed in Table 1.

Social and economic disparities existed between male and female respondents. Men were more likely to live with a spouse (69% vs. 46% of women; p=0.001) and women were more likely to live alone (21% vs. 9% of men; p=0.01). A greater percentage of men had household income >$35,000/year than women (63% vs. 49% of women; p=0.05). A far greater portion of female respondents (46%) lived in a household with income <$35,000/year than the general U.S. population (21%).
Duration of HF diagnosis correlated with both age and economic status. Respondents with HF duration <1 year consisted predominantly of those in the 50-59-year-old age group (67%). Patients with HF duration >5 years largely comprised those age ≥60 years (59%). Full-time employment decreased from 39% at <1 year of HF duration to 13% at >5 years of HF duration, which negatively correlated with duration of HF diagnosis (r= –0.154; p=0.005).
This negative correlation remained even after adjusting for age, making HF duration a separate and independent contributor to loss of full-time employment in addition to age. Combined retirement and disability status grew from 42% to 69% from <1 year to >5 years of HF duration. The portion of patients using Medicare increased from 25% to 63% from <1 year to >5 years of HF duration.
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Self Care, Medication Adherence, Patient Discharge, Diuretics, Ambulances, Body Weight, Weight Gain, Hospitalization, Heart Failure, Fatigue, Anxiety
< Back to Listings