Is TMVR Following ELASTA-Clip Safe and Effective?
Electrosurgical leaflet laceration and stabilization of the implant (ELASTA-Clip) followed by transapical transcatheter mitral valve replacement (TMVR) is a feasible and less invasive option for management of failed mitral transcatheter edge-to-edge repair (M-TEER) that can be performed with acceptable results in a selected patient population, according to a new study published in JACC: Cardiovascular Interventions.
In the multicenter retrospective study, Daryoush Samim, MD, et al., collected data from eight centers in four countries on 22 patients (mean age 77.8 years; 40.9% women) at high surgical risk (mean EuroSCORE II 8.0; mean STS score 7.2%) with symptomatic failed M-TEER defined as persistent or recurrent mitral regurgitation (MR) (n=21 with MR ≥3+) or iatrogenic mitral valve (MV) stenosis (n=1), who underwent the ELASTA-Clip procedure (20 transseptal, 2 transapical) followed by successful transapical TMVR.
The ELASTA-Clip intervention was successful in all patients. And it was considered a technical success in 21 patients (as defined by Mitral Valve Academic Research Consortium criteria) without left ventricular outflow tract obstruction or conversion to sternotomy.
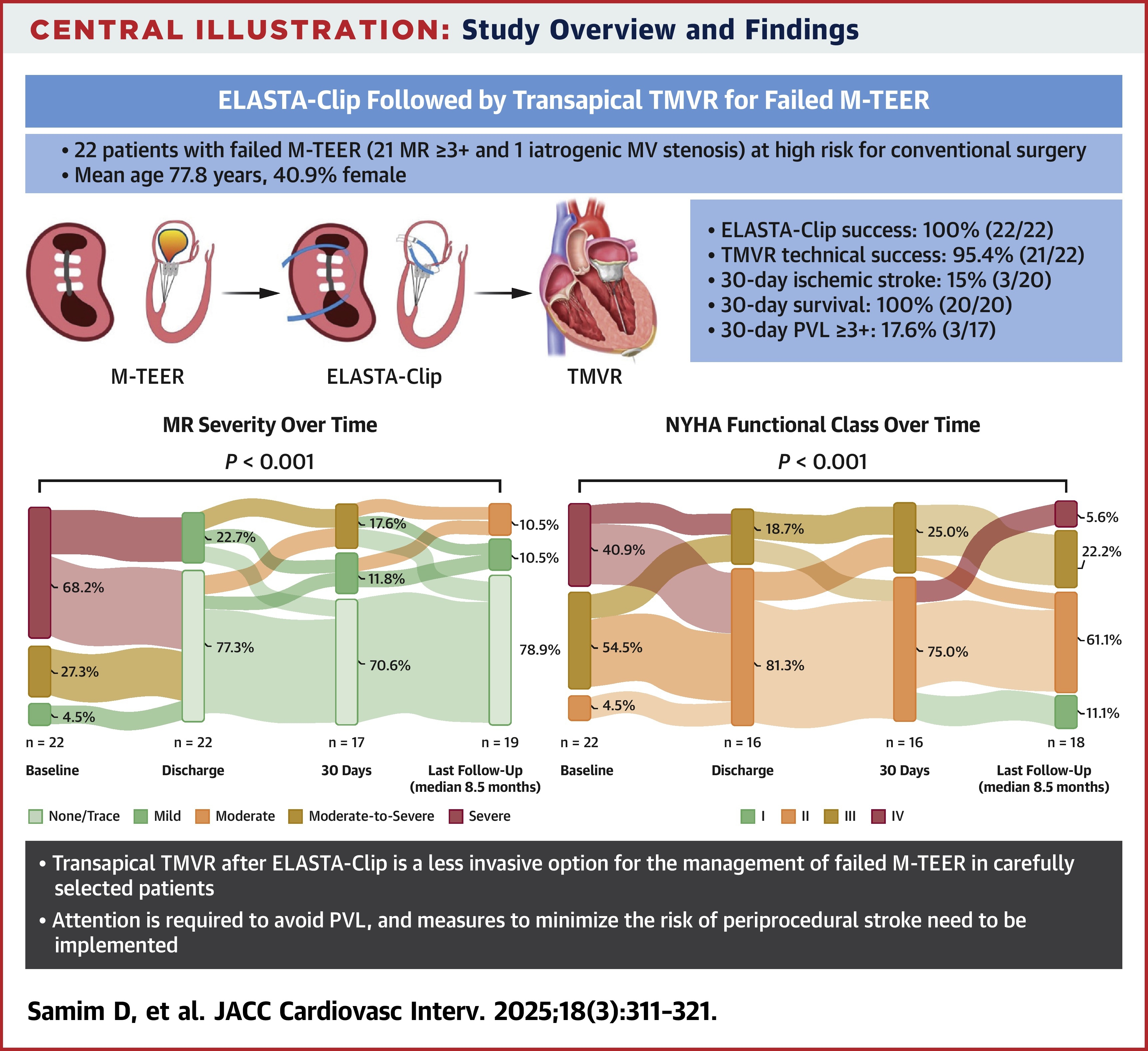
Results showed that at 30 days follow-up, 20/20 patients were alive. Three patients had been rehospitalized for heart failure (uncontrolled atrial fibrillation in two cases) and one had undergone a reintervention of valve retensioning.
Three patients experienced paravalvular leak progression and three ischemic stroke. Of the 21 with MR≥3+, MR was reduced to grade 1+ or less in all patients with durable results (89.5% [17/19], p<0.001) at last follow-up. NYHA functional class also significantly improved to ≤II in 13/16 (81.3%) at discharge (p<0.001) and 13/18 at last follow-up (72.2%; p<0.001).
Of the 13 patients who had one-year follow-up, four died (three from noncardiovascular causes).
While concluding that TMVR after ELASTA-Clip is feasible and less invasive, the authors add that, "Particular attention is required to avoid paravalvular leakage and measure to minimize the risk of periprocedural cerebrovascular events need to be implemented in future larger-scale prospective studies with longer term follow-up."
In an accompanying editorial comment, Paolo Denti, MD, also notes the significant stroke incidence of 15%, and that only five of the patients had a periprocedural cerebrovascular protection device. "These data raise awareness that percutaneous electrosurgery generates ash, and this could have a role in the incidence of thromboembolic events," he writes. "Paramount importance must be dedicated to mitigating the risk of cerebrovascular events."
Clinical Topics: Heart Failure and Cardiomyopathies, Valvular Heart Disease, Acute Heart Failure
Keywords: Mitral Valve Stenosis, Electrosurgery, Heart Failure
< Back to Listings

