Focus on EP | A Practical Primer For the 2023 AFib Guideline

One of my New Year's resolutions was to read the entire 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation (AFib).1 This was no small task given the tremendous amount of AFib-related research that had accumulated since the 2014 AFib guideline (only 76 pages) and the subsequent 2019 AFib guideline focused update (only 29 page).2,3
After reading all 171 pages of the 2023 AFib guideline, here are seven clinically-relevant highlights. This is not meant to be an exhaustive review and I encourage everyone to read more about these specific topics in the guideline. And don't stop there… the entire guideline is a good read.
AFib Is Not a Black and White Condition
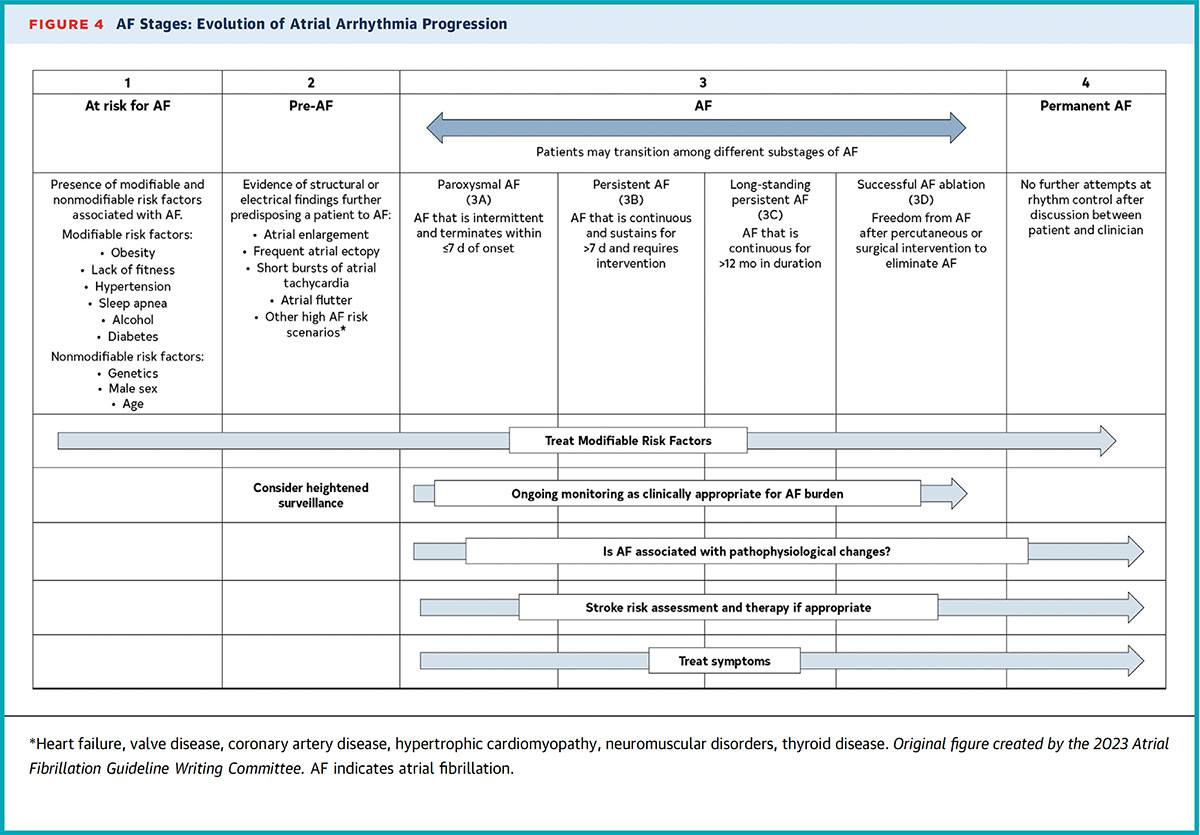
AFib was once thought of as a condition that was either present or absent and with a disease severity relegated to discrete states (paroxysmal, persistent, etc.). As with heart failure, we now acknowledge that AFib exists on a continuum, beginning in patients who are at-risk but without overt features (Stage 0) and eventually progressing to a permanent state (Stage 4) (Figure 1).
I'm hopeful that the newfound appreciation for AFib as a dynamic disease will eventually lead to a more nuanced definition of AFib ablation outcome, rather than the current "successful or not" definition. The goal of ablation is to reduce AFib burden and interrupt its progression. The new AFib staging system in the guideline acknowledges the impact of ablation on disease modification by assigning it a unique stage (Stage 3D).
Manage AFib With Consumer Devices
The AppleWatch became the first consumer device to detect AFib approved by the U.S. Food and Drug Administration, in 2018, and now there are more than a half a dozen AFib monitoring devices. The 2023 AFib guideline recommends the use of consumer devices with high-quality tracings to monitor AFib recurrence in patients with known AFib.
Interestingly, this Class 2a recommendation carries the same strength as the recommendation for the use of cardiac implantable electronic devices (CIEDs), including pacemakers, defibrillators and loop recorders, for monitoring AFib burden, despite the obvious differences in detection accuracy between consumer devices and CIEDs.
Anticoagulants, Yes. Antiplatelets, No (Mostly)
Four Key Takeaways
- Consider anticoagulation even in patients with lower risk AFib.
- Sinus rhythm maintenance is the priority.
- Catheter ablation is the preferred treatment in many AFib populations.
- Left atrial appendage occlusion is reasonable as a patient preference.
Click here to access the AFib Guideline Hub for tools and resources to implement the guideline recommendations – as well as the complete guideline.
The threshold to anticoagulate continues to be lowered. It is even more reasonable (recommendation upgrade from Class 2b in 2019 to Class 2a in 2023) to pursue anticoagulation in men with a CHA2DS2-VASc score of 1 and in women with CHA2DS2-VASc score of 2, which is equivalent to an intermediate annual stroke risk of 1-2%.
In these individuals, stroke risk reduction can be further supported by using stroke risk models such as ATRIA (which incorporates age >85 and renal disease) and GARFIELD (which additionally incorporates active smoking and dementia).
Antiplatelet use is now discouraged for stroke risk reduction in the AFib population. However, antiplatelets should be continued for patients with other indicated conditions (coronary artery disease, peripheral artery disease, etc.).
Sinus Rhythm For All
With this new guideline, the question has shifted from "who should have sinus rhythm maintained," to "who should not have sinus rhythm maintained." This is a major paradigm change from the previously favored rate-control strategy, which I've viewed as a more palliative approach to AFib management that treated symptoms and heart rate rather than the disease itself.
The 2023 AFib guideline recognizes the myriad clinical benefits associated with sinus rhythm maintenance, which includes risk reductions in mortality, stroke, hospitalization, dementia and worsening cardiac structural abnormalities. Even for those patients with AFib who claim to be asymptomatic, we should strive to maintain sinus rhythm.
Despite these strong recommendations for rhythm control ranging from Class I to Class 2b, I suspect clinical adoption will be slow. It may be challenging for cardiologists to convince their established AFib patients, who were previously managed with a rate control strategy, to accept a new rhythm control plan.
Catheter Ablation is the Way
Just as rhythm control is now preferred over rate control as the AFib treatment strategy, catheter ablation is now preferred over antiarrhythmic drugs as the treatment modality to maintain sinus rhythm.
In the new guideline, catheter ablation is notably endorsed in symptomatic AFib patients in whom antiarrhythmic drugs are not preferred (Class I); as first-line therapy in younger patients with few comorbidities who have symptomatic paroxysmal AFib (Class I); as first-line therapy in patients (other than younger with few comorbidities) with symptomatic paroxysmal or persistent AFib (Class 2a); and even in asymptomatic or minimally symptomatic AFib patients (Class 2b).
Of note, catheter ablation for symptomatic AFib patients is also viewed as having greater economic value than antiarrhythmic drugs.
Additionally, the recommended primary lesion set in catheter ablation is pulmonary vein isolation (PVI) unless a discrete arrhythmia focus is identified (Class I). There is unclear value in ablation of additional areas beyond PVI, such as the posterior wall, low voltages areas, fractionated signals, etc. (Class 2b).
LAAO Gains Momentum
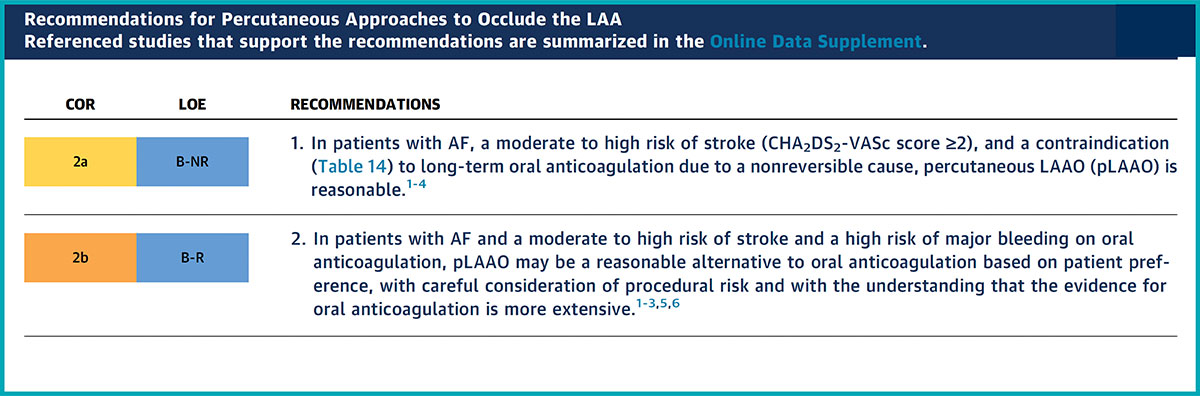
Percutaneous left atrial appendage occlusion (LAAO) was first recognized in the 2019 ACC/AHA AFib guideline as a Class 2b recommendation in AFib patients with increased risk of stroke who have contraindications to long-term anticoagulation. Now this recommendation has been upgraded to Class 2a for this patient population.
Furthermore, in the 2023 AFib guideline, there are two new Class 2b recommendations for LAAO: patients with a history of major bleeding on anticoagulation who prefer LAAO as an alternative to long-term anticoagulation and patients with conditions associated with high risk of recurrent intracranial hemorrhage.
With the broadened indications for stroke risk reduction in AFib, along with the iterative improvements in the safety and efficacy of newer generation LAAO devices, it's conceivable that with time the class of recommendation could be upgraded for LAAO.
Cardiac Surgery Does Have a Role
Successful management of AFib often necessitates a multidisciplinary approach, which may include surgical ablation and/or LAA exclusion. For AFib patients who are undergoing cardiac surgery for another condition, surgical LAA exclusion is indicated to reduce stroke risk (Class I, if CHA2DS2-VASc score ≥2) and surgical ablation can be helpful to reduce AFib recurrence (Class 2a). In patients with symptomatic, persistent AFib refractory to antiarrhythmic drugs, standalone hybrid epicardial and endocardial ablation may be reasonable to reduce AFib recurrence (Class 2b).
Notably, continued anticoagulation is recommended even after surgical LAA exclusion is performed. The stroke risk reduction achieved by surgical LAA exclusion alone is uncertain.
Where Do We Go From Here?
Although the new AFib guideline is impressive in scope, it nonetheless reflects a static snapshot of the AFib landscape up to November 2022. New research findings continue to challenge our current understanding of AFib, and novel treatments, such as pulse field ablation, have since emerged that will undoubtedly influence future recommendations for care.
While we should embrace and endorse the significant guideline updates in AFib management, we must remember that patients with complex disease, late-breaking research, and innovative technologies will always fall outside even the most recent clinical recommendations.

This article was authored by Edward Chu, MD, FACC (@Ed_Chu_MD), an electrophysiology attending physician in Miami, FL.
References
- Writing Committee Members; Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation. J Am Coll Cardiol 2024;83:109-279.
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol 2014;64:e1-76.
- January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol 2019;74:104-32.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Heart Failure and Cardiomyopathies, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure
Keywords: Cardiology Magazine, ACC Publications, Atrial Fibrillation, United States Food and Drug Administration, Anticoagulants, Pacemaker, Artificial, Heart Failure