Cover Story | Clinical Decision-Making in Aortic Stenosis in Patients With Bicuspid Valves

In the past decade, the U.S. has seen a 25-fold increase in the use of TAVR, with more than 100,000 performed annually. This technique is now employed in approximately 85% of all isolated aortic valve replacements. Despite this growth, there are notable gaps in the evidence. First, around 10% of TAVR procedures are performed on patients with bicuspid aortic valves (BAVs), yet no clinical trial data exist comparing TAVR vs. surgical aortic valve replacement (SAVR).
Additionally, the bulk of the evidence supporting TAVR comes from its application in older patients over the age of 65 years, who have a relatively short life expectancy. Concerns regarding the long-term durability of bioprostheses, especially regarding how to manage younger patients throughout their lifetimes, remain to be addressed.
"The evidence of benefit in any study is limited to the population in which it was studied in the trials," says Michael J. Mack, MD, MACC, chair of the cardiovascular service line for Baylor Scott & White Health and chair of BSW The Heart Hospital – Plano Research Center in Texas.
In an interview with Cardiology, he notes that even in the low-risk trials of TAVR vs. SAVR, no patients were under the age of 65, and only about 9% were below 70. Mack also notes that the younger the patient with severe aortic stenosis (AS), the more likely it is that they'll have a bicuspid aortic valve, "which we haven't really studied at all."
Given these notable gaps in the evidence, how should clinicians approach the management of younger patients with BAV and severe AS?
Bicuspid Aortic Valve 101
BAV is the most common congenital heart defect, affecting up to 2% of the population, with about a 3:1 predominance in men. Clinical manifestations include AS or regurgitation and infective endocarditis. Many patients with BAV also have an associated aortopathy that can lead to development of an aortic aneurysm or dissection.
AS is the most common clinical manifestation of BAV, where abnormal leaflet architecture leads to altered flow and increased mechanical stress on the leaflets. Over time, this stress leads to premature valve degeneration, similar with that seen in tricuspid valves, but occurring at an accelerated rate.
– Michael J. Mack, MD, MACC
The majority of BAVs function normally in childhood, although a small proportion do experience valve dysfunction in adolescence or at a very young age.
The most common clinical scenario for patients with BAV is the development of calcific AS later in life, typically presenting as severe AS after the age of 50. While AS secondary to BAV develops and progresses at variable rates, patients experience rapid progression.
The SAVR Zone
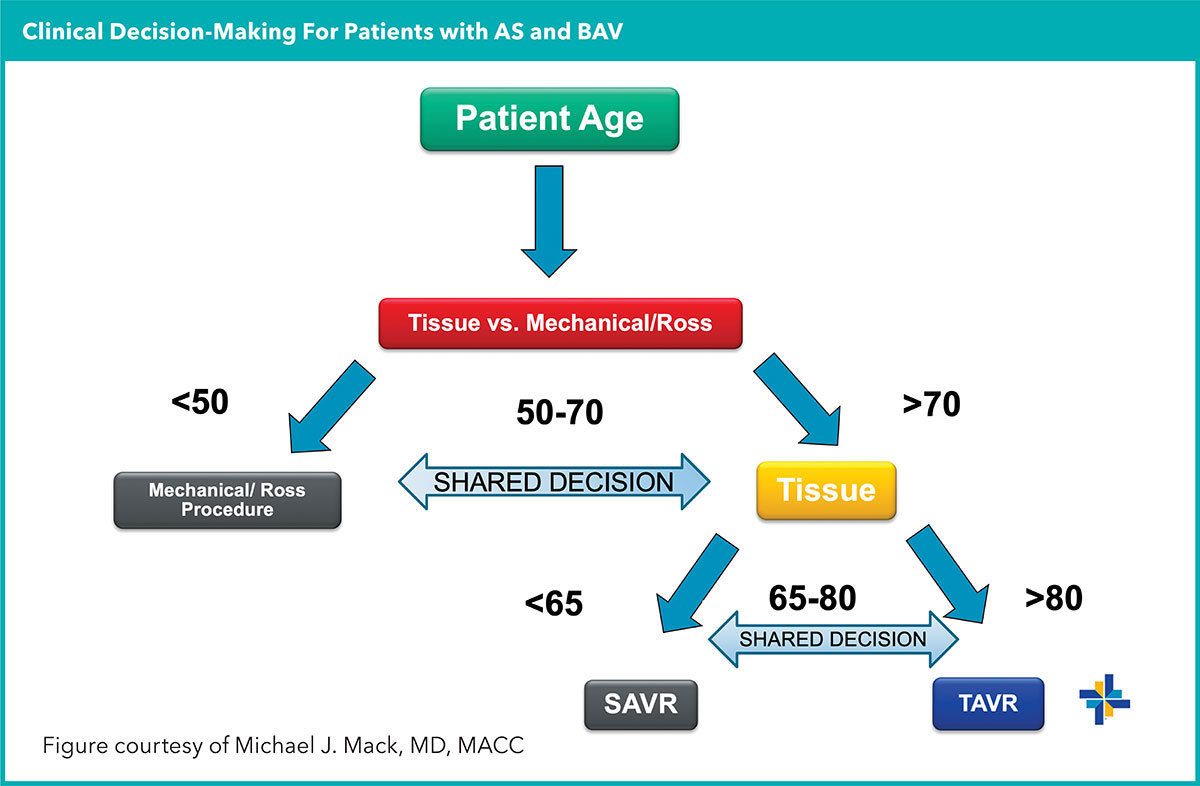
In the 2020 ACC/AHA guideline for valvular heart disease, mechanical valve prostheses are recommended for patients under 50 years of age unless there is a contraindication to oral anticoagulation with a vitamin-K antagonist, in which case a bioprosthesis can be considered.1 Between the ages of 50 and 65, the guideline suggests that either a mechanical or bioprosthetic valve is reasonable "with consideration of individual patient factors and after informed shared decision-making."
SAVR for AS in a young patient is a procedure that offers excellent short-term and mid-term outcomes. However, the trauma and extended recovery from surgery and lifetime oral anticoagulation are difficult pills to swallow. Additionally, despite low operative morbidity and mortality, valve degeneration and reintervention are concerns. Only patients who undergo the Ross procedure appear to gain back a life expectancy similar with the general population (see sidebar).
"For a patient under 55 years old with a BAV and AS, the discussion should mainly be about the different surgical options, and this is clearly reflected in the guideline," says David J. Cohen, MD, MSc, director of clinical and outcomes research at the Cardiovascular Research Foundation in New York and director of academic affairs at St. Francis Hospital in Roslyn, NY.
"The younger the patient, the more likely it is they should probably undergo surgery and receive a mechanical valve or a Ross procedure," Mack agrees.
The management of asymptomatic patients is the subject of ongoing study, with at least one trial demonstrating a survival advantage from early surgery compared with "watchful waiting." Asymptomatic AS in BAV can be tricky, says Mack. "It has always amazed me how often patients with severe AS and bicuspid valves are asymptomatic. It's probably because they've had it for years and years and they've slowly adapted to it."
According to Mack, a "not unusual story" is a 55-year-old guy who does hundred-mile bike rides on weekends, has a bicuspid valve and severe AS, and hasn't slowed down at all. "We put him through surgery and six weeks later when I ask if he feels any better, he tells me he feels exactly the same as he felt before," he says.
The Shared Decision-Making Zone
Broadly speaking, in the current guidelines TAVR is favored in older patients while SAVR is recommended more in younger patients.
While TAVR is indicated for the treatment of patients 65 years and older with symptomatic AS regardless of surgical risk, the indication for TAVR is silent on the issue of whether the native aortic valve has a bicuspid or tricuspid configuration.
Guidelines are also silent on indications for TAVR in people <65 years old (<75 in the 2021 ESC/EACTS guideline). Nonetheless, there are an increasing number of AS patients (with and without BAV) under 65 receiving TAVR.
– David J. Cohen, MD, MSc
In administrative data presented at the Society of Thoracic Surgeons conference in January 2024, 22% of patients who were ≤60 years old treated for AS in California between 2013 and 2021 received TAVR instead of a surgical approach, with a steady annual increase in the use of TAVR.2 By 2021, nearly half of patients ≤60 years in this cohort were receiving TAVR rather than SAVR.
"As cardiac surgeons, we owe it to our patients to take a more prominent role in providing the highest quality evidence to help our patients make these major health care decisions," said the paper's senior author, Joanna Chikwe, MD, FACC, chair of cardiac surgery at the Smidt Heart Institute at Cedars-Sinai in Los Angeles, CA, in a press release.
"While transcatheter therapy appears more attractive to most patients, there are clearly long-term benefits with surgical therapy for the lifetime management of valvular heart disease in many patients," she said." Chikwe stressed the need for randomized trials and "more balanced and informed patient-centered decision-making to support more appropriate practice in this younger patient population."
Playing the Long Game
Treating younger patients with BAV and AS requires long-term thinking. "If a patient in their 50s needs an aortic valve procedure for AS, it's likely they'll need three valves through their lifetime, assuming they have an average of 30 years to live," explains Mack.
"Somewhere in those three valves, there will have to be a surgical valve implanted. Maybe you can do a TAVR first and then a valve-in-valve TAVR second, but it will be unlikely you can do three TAVRs."
Mack cautions against having surgery as the third procedure given that patients will likely be in their late 70s or 80s and in far worse health than in their 50s or 60s. "You'll have to explant two TAVR valves to implant a surgical valve," he says.
This is where shared decision-making comes in. "These days everyone is coming in asking for TAVR and many of them will get it. But if these patients are younger, it's a more complicated decision. Sure, TAVR will get you back on your feet more quickly, but there may be some trade-offs," says Cohen.
While there have been no trials comparing TAVR to SAVR in patients with bicuspid AS, a number of observational studies of highly selected patients with bicuspid AS undergoing TAVR have reported favorable outcomes comparable with those seen in tricuspid AS treated with TAVR or bicuspid AS treated with SAVR.3
"Under circumstances where the BAV anatomy is favorable for TAVR and transfemoral access is feasible, successful implantation of a transcatheter heart valve offers clinical outcomes that are comparable with SAVR," says Stephan Windecker, MD, chair of cardiology at Bern University Hospital, Inselspital, Switzerland. "Conversely, where the aortic valve anatomy is unfavorable or femoral access is not adequate, SAVR remains the treatment of choice."
With no randomized data comparing the two options in patients with BAV stenosis, it is unknown whether TAVR has the same favorable outcome as SAVR in patients with tricuspid valve disease, says Windecker. "Specifically, the procedural risks of annular rupture, stroke and, importantly, paravalvular leak may be higher in bicuspid compared with tricuspid anatomy using TAVR."
"Observational studies to date indicate that TAVR in selected patients with bicuspid valve disease performs well, but validation in a randomized clinical trial against the current gold standard SAVR is missing," says Windecker.
Other longer-term questions with TAVR in younger patients revolve around durability and repeatability. Given that regardless of the valve chosen, most patients in their 50s or early 60s will likely need a second procedure at some point (or maybe even a third), there is limited evidence to suggest that one kind of bioprosthesis – surgical or transcatheter – has better durability than the other.
With the currently available data – again, derived almost exclusively from patients with tricuspid valves – valve durability appears to be similar for TAVR and SAVR bioprostheses, with both options offering less durability than mechanical SAVR valves.
"I'm comfortable saying the TAVR and SAVR bioprostheses are durable out to somewhere between five to 10 years at this point. But we have zero comparative information in bicuspid valve patients, and we know the native bicuspid valve can influence TAVR valves' deployment and expansion," says Mack.
"Yet, we do know that surgical valves degenerate more quickly in patients who are younger, so this is a concern when we look at applying TAVR to younger patients," he adds.
– Stephan Windecker, MD
Windecker also notes that, "TAVR prostheses implanted into bicuspid anatomy may behave differently. "Noncircular expansion may constitute a risk for valve degeneration or subclinical valve thrombosis," he says. "Moreover, there may be progression of aortopathy over time requiring surgery of the ascending aorta at a later point in time."
There may also be benefit to removing the bicuspid valve early on. TAVR essentially involves putting a round peg in an irregular oval hole, while surgical replacement removes the anatomically suboptimal valve permanently.
"Many times, stenotic bicuspid valves have very bulky calcified leaflets and with TAVR it can be hard to push that all aside and get expansion of the valve," says Cohen. "Also, when you leave the leaflets behind because you're doing a TAVR not a SAVR, they're going to interact with the valve frame and may exert forces that impact valve durability."
Anatomical risk stratification based on the device implantation zone is one of the central considerations in patient selection for either procedure, says Windecker. "There is a wide spectrum of this disease, and certainly we already know there are some patients who are very well suited for TAVR and others who are not. But it's highly selected and we are less certain across the entire range."
Bicuspid patients with both a calcified raphe and bulky, eccentric calcification are not considered good candidates for TAVR.
BAV Randomized Trials in the Works
Since TAVR is approved for patients with bicuspid valve disease despite there being no randomized data to support it, industry has, unsurprisingly, not taken the initiative in conducting comparative trials. However, there are three investigator-led trials in the works that will compare TAVR and SAVR specifically in these patients.
The NAVIGATE trial (chaired by Windecker and Matthias Siepe, MD) and the BELIEVERS trial (chaired by Raj R. Makkar, MD, FACC, and Vinod H. Thourani, MD, FACC) will both randomize patients with severe bicuspid AS to TAVR or SAVR, with a determination for eligibility made by committee.
The trials will also follow those for whom the local heart team felt there was not equipoise in parallel, prospective registries according to the treatment selected. A third trial, called YOUNG TAVR (chaired by Mayra E. Guerrero, MD, FACC, and Thourani), will look at TAVR (vs. SAVR) in younger patients with either bicuspid and tricuspid valves.
NAVIGATE will assess the primary safety endpoint of death, stroke and moderate or more paravalvular regurgitation at one year, as well as the primary efficacy endpoint of death, stroke and procedure- and valve-related hospitalizations at five years, with pre-specified follow-up at 10 years. Patients will be asked for lifelong follow-up.
"The critical thing about these trials, and hopefully they'll all get funded, is that we'll follow patients for 10 and maybe 20 years and better understand durability. We'll also see outcomes in the patients who were not eligible for randomization," says Cohen, an investigator for the BELIEVERS trial.
"We need to see what happens and how decisions are made for people who are on the higher end of the surgical risk spectrum where they're likely to get TAVR," says Cohen. "We also need to see this for patients who are lower risk and have anatomy not suitable for TAVR who are sent for surgery. Seeing the whole picture is going to be very valuable and help inform how to tailor treatment for this group of patients with BAV and AS."
Only Ross Restores Life Expectancy
The Ross procedure is emerging as the optimal surgical treatment for younger adults with aortic valve disease, with a growing number of studies now showing it is the only surgical option that restores normal life expectancy to a patient.1,2
First described by Donald Ross, MD, in 1967, the procedure involves replacing a diseased aortic valve with the patient's own pulmonary valve (autograft). The pulmonary valve is then replaced with a donor valve (homograft) in the pulmonary position. This approach leverages the pulmonary valve's natural durability and biocompatibility compared to artificial prostheses, eliminating the need for lifelong anticoagulation therapy.
The Ross procedure is neither infallible nor permanent: failure is most often related to regurgitation of the neoaortic valve in the second decade after surgery. As well, up to half of pulmonic homograft valves require reintervention within 10 to 20 years. "The procedure was popular in the 90s but fell out of favor because it's a very complex operation and there were some unfortunate outcomes because not everyone who was doing the procedure should have been," says Mack.
"Lately, there is renewed interest in making the Ross procedure more widely available again and maximizing outcomes by properly training surgeons, mentoring surgeons, and so on. I think it will receive wider adoption this time," he adds.
Mack estimates that in 2023 <1% of the aortic valve surgeries done on BAVs in the U.S. were Ross procedures. The Ross is typically reserved for younger patients with appropriate anatomy and tissue characteristics in whom anticoagulation is either contraindicated or undesirable and should only be performed by surgeons experienced in the procedure.
In one retrospective analysis of 225 adult patients (mean age, 42 years) who underwent the Ross procedure at Baylor Scott & White, overall survival at one, 10 and 20 years was 97.8%, 94.2% and 81.3%, respectively, approximating that of the general population (log-rank p=0.32).1 The need for reintervention increases steadily during the second decade after the Ross procedure, but less than half of patients require any reintervention for up to 20 years.
In a study comparing young and middle aged adults (median age, 41 years) who received either the Ross or a mechanical aortic valve replacement for severe aortic stenosis, Gofus, et al., found that the two operations offered similar operative risk and similar risk of reoperation.3 Over an average follow-up of 4.1 vs. 6.1 years, the Ross group had lower all-cause mortality (0.7% vs. 6.5%; p=0.015), and this result remained significant even when looking at only cardiac- and valve-related deaths only (p=0.048).
Unlike the Ross group, patients who received mechanical valves had significantly lower relative survival compared with the age- and sex-matched general population, leading Gofus, et al. to conclude that the Ross procedure be the preferred treatment option for young and middle-aged adults with aortic valve disease in specialized centers.
References
- Ryan WH, Squiers JJ, Harrington KB, et al. Long-term outcomes of the Ross procedure in adults. Ann Cardiothorac Surg 2021;10:499-508.
- Shih E, Ryan WH, Squiers JJ, et al. Outcomes of the Ross procedure in patients older versus younger than 50 years old. Eur J Cardio-Thorac Surg 2023;64:ezad260.
- Gofus J, Fila P, Drabkova S, et al. Ross procedure provides survival benefit over mechanical valve in adults: A propensity-matched nationwide analysis. Eur J Cardio-Thorac Surg 2022;61:1357-65.
Supporting Patient Conversations
Visit CardioSmart.org/topics/aortic-stenosis to download these infographics and more to support the crucial shared decision-making conversations with patients.

This article was authored by Debra L. Beck, MSc.
References
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease. J Am Coll Cardiol 2021;77:e25-e197.
- The Society of Thoracic Surgeons. Almost 50% of Patients Under 60 Years Choose TAVR Over SAVR with Worse Outcomes. Accessed Feb. 25, 2024. Available here.
- Windecker S, Okuno T, Unbehaun A, et al. Which patients with aortic stenosis should be referred to surgery rather than transcatheter aortic valve implantation? Eur Heart J 2022;43:2729-50.
Clinical Topics: Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Invasive Cardiovascular Angiography and Intervention, Valvular Heart Disease, Aortic Surgery, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Interventions, Interventions and Structural Heart Disease
Keywords: Cardiology Magazine, ACC Publications, Bicuspid Aortic Valve Disease, Transcatheter Aortic Valve Replacement, Aortic Valve Stenosis, Endocarditis, Aortic Valve, Mitral Valve