Competency-Based Advancement Program Improves Nursing Retention in a CV ICU
Quick Takes
- In the cardiovascular (CV) intensive care unit (ICU), the retention of skilled nurses plays an important role in quality care delivery.
- Despite nursing shortages during the pandemic, the implementation of nontraditional advancement strategies that focus on professional-based competencies has the potential to increase nursing retention rates and ultimately improve care.
Introduction
In the CV ICU, delivery of quality critical care involves a multidisciplinary team of specialized CV health care professionals. In addition to standard ICU skills, CV ICU nurses have expanded responsibilities and skills that require specific education and investment beyond what is learned in nursing school. As such, the hiring, education, and retention of CV ICU nurses is an important part of improving care delivery for this complex patient population. In the face of increased nursing shortages during the coronavirus disease 2019 pandemic, the implementation of nontraditional career and salary advancement strategies that focus on professional-based competencies has the potential to increase nursing retention rates and ultimately improve care.
Critical Care Nursing Retention: Driving Factors
Nursing retention in the critical care space is a globally recognized health care challenge. Turnover and shortages often disproportionately affect critical care units, and this has only been underscored by the current global pandemic.1,2 The demand for nurses is estimated to increase exponentially in the United States, but a recent study found intent to leave—a marker for nursing turnover—to be as high as 33% across ICU nurses nationally.3,4 Job satisfaction, training opportunities, and work environment are among significant drivers of intent to leave,5-8 and a recent study examining nursing work environments found that meaningful recognition for nurses was ranked as a top reason to reconsider intent to leave.4 The American Society of Critical Care Nurses has included this metric in its standards for nearly two decades.9
Improving CV ICU Nursing Retention: Our Experience
The American Heart Association has recognized the CV ICU as increasingly complex and requiring specific policies, practices, and procedures beyond that of a typical ICU.10 However, there is a dearth of research about the unique role of the CV ICU nurse and even less regarding CV ICU-specific nursing best practices or education.
Our unit is a tertiary care, 16-bed CV ICU located in a 500-bed urban hospital in the Midwest that utilizes a multidisciplinary staffing model led by dedicated cardiac intensivists and cardiac surgeons. The unit sees more than 1,000 individual CV ICU admissions each year, including perioperative cardiac surgery patients, advanced heart failure patients, a robust left ventricular assist device patient population, and those requiring temporary mechanical circulatory support. In 2017, retaining a core team of dedicated CV ICU nurses was identified as an area of improvement for our unit and hospital. A philanthropic donation to the hospital was directed at this aim, with the goal of decreasing nursing attrition by 50% in 2 years' time.
Prior to our intervention, professional advancement in the CV ICU was achieved through a hospital-wide program based on traditional metrics including professional membership, nursing degrees, unit leadership, projects, and education. Our team established a formal CV ICU clinical advancement program based on unit-specific clinical competency and cardiac-focused educational achievements. Our aim was to reinvent the way nurses progressed through their career, encouraging unit-level engagement with a focus on promoting and improving CV ICU-specific professional practice and competency. Our hope was that this intervention would increase nursing engagement and job satisfaction, with a subsequent improvement in CV ICU nursing retention.
Over several years, specific interventions were implemented in our unit to this aim. Unit renovations included the creation of a state-of-the-art media room with conferencing technology that would facilitate nursing education and provide a central space for collaborative meetings and presentations. A new position was created for CV ICU Clinical Nurse Leader to improve evidence-based practice throughout the unit, in addition to the hiring of a dedicated cardiac intensivist unit director passionate about nursing education and nursing involvement with didactic education on rounds. The new pathway tied increased compensation and promotion to demonstration of CV ICU-specific competencies, such as open-heart recovery and management of mechanical circulatory support devices, unit tenure, and the ability to "coach" newly hired nurses. Additional involvement in unit-specific quality, performance, or educational initiatives was also included. This was achieved through in-services and dedicated educational sessions for which nurses also gained continuing education credits.
Using a point-based system, compensation was calculated based on the factors noted above. All nurses were trained along a specific skill trajectory and could anticipate the time it would take to achieve certain competencies. Competency and readiness for additional training was assessed by the unit management and educator. Credentialing, certifications of competency, and professional society memberships were subsidized by the philanthropic funds, with a sustainability plan to continue the program for years to come.
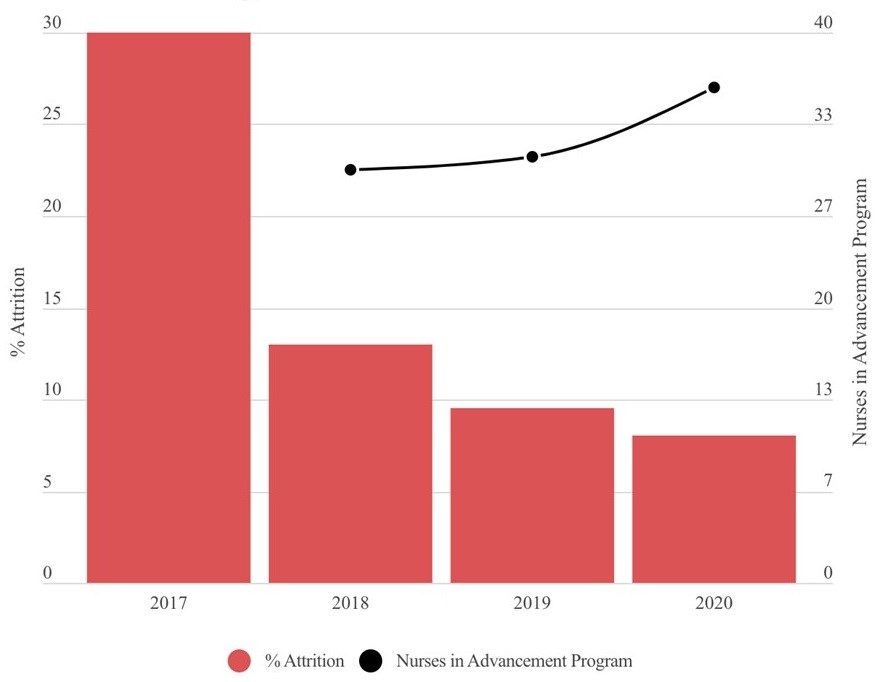
Prior to this intervention, nursing turnover in the unit for fiscal year 2017 was 30%. In the subsequent 3 years, nursing attrition decreased to 13%, 9.5%, and 8%, respectively (Figure 1), with an absolute reduction of 73%. During this time, the CV ICU case mix index—a marker of patient acuity and complexity—increased from 5.1 to a unit record of 6.4, which was more than twice that of our hospital's other ICUs. During the same time, our patient volume increased by 49%. Despite this consistent increase in volume and acuity and the strains of a global pandemic, our nursing attrition rates remain low and reported job satisfaction high.
Figure 1: Nursing Retention in the CV ICU
Conclusion
Tenured and skilled CV ICU nurses are integral parts of care delivery. Nursing turnover persists as a national multifaceted issue. In our complex and busy CV ICU, the implementation of a competency-based professional advancement program with a focus on clinical nursing education, unit-based competencies, and professional development dramatically improved nursing retention despite an increase in volume and acuity.
References
- Sawatzky JAV, Enns CL, Legare C. Identifying the key predictors for retention in critical care nurses. J Adv Nurs 2015;71:2315-25.
- NSI Nursing Solutions. 2021 NSI National Health Care Retention & RN Staffing Report (www.nsinursingsolutions.com). March 2021. Available at: https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf. Accessed July 19, 2021.
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, National Center for Health Workforce Analysis. Supply and Demand Projections of the Nursing Workforce: 2014-2030 (https://bhw.hrsa.gov). July 21, 2017. Available at: https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nchwa-hrsa-nursing-report.pdf. Accessed July 19, 2021.
- Ulrich B, Barden C, Cassidy L, Varn-Davis N. Critical Care Nurse Work Environments 2018: Findings and Implications. Crit Care Nurse 2019;39:67-84.
- Halter M, Boiko O, Pelone F, et al. The determinants and consequences of adult nursing staff turnover: a systematic review of systematic reviews. BMC Health Serv Res 2017;17:824.
- Labrague LJ, De Los Santos JAA, Falguera CC, et al. Predictors of nurses' turnover intention at one and five years' time. Int Nurs Rev 2020;67:191-8.
- Khan N, Jackson D, Stayt L, Walthall H. Factors influencing nurses' intentions to leave adult critical care settings. Nurs Crit Care 2019;24:24-32.
- Gebregziabher D, Berhanie E, Berihu H, Belstie A, Teklay G. The relationship between job satisfaction and turnover intention among nurses in Axum comprehensive and specialized hospital Tigray, Ethiopia. BMC Nurs 2020;19:79.
- American Association of Critical-Care Nurses. AACN Standards for Establishing and Sustaining Healthy Work Environments: A Journey to Excellence. 2nd ed. Aliso Viejo, CA: American Association of Critical-Care Nurses; 2016.
- Fordyce CB, Katz JN, Alviar CL, et al. Prevention of Complications in the Cardiac Intensive Care Unit: A Scientific Statement From the American Heart Association. Circulation 2020;142:e379-e406.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, COVID-19 Hub, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Cardiac Surgery and Heart Failure, Acute Heart Failure, Mechanical Circulatory Support
Keywords: Critical Care Nursing, Leadership, Clinical Competence, Schools, Nursing, Heart-Assist Devices, Coronavirus, Fund Raising, Benchmarking, American Heart Association, Tertiary Healthcare, Pandemics, COVID-19, Quality Improvement, Education, Nursing, Critical Care, Intensive Care Units, Workforce, Education, Continuing, Credentialing, Certification, Educational Status, Educational Status, Heart Failure, Salaries and Fringe Benefits, Evidence-Based Practice, Patient Acuity, Cardiac Surgical Procedures, Hospitals, Urban, Diagnosis-Related Groups, Reference Standards, Patient Care Team
< Back to Listings