LBB Area Pacing for Cardiac Resynchronization Therapy
Quick Takes
- Conduction system pacing can restore the electromechanical dyssynchrony induced by left bundle branch block (LBBB) or chronic conventional permanent ventricular pacing.
- Left bundle branch area pacing (LBBAP) is safe and feasible and has been associated with significant QRS narrowing and improvement of left ventricular ejection fraction (LVEF) in patients with cardiac resynchronization therapy (CRT) indications.
- LBBAP can be an alternative pacing strategy for CRT.
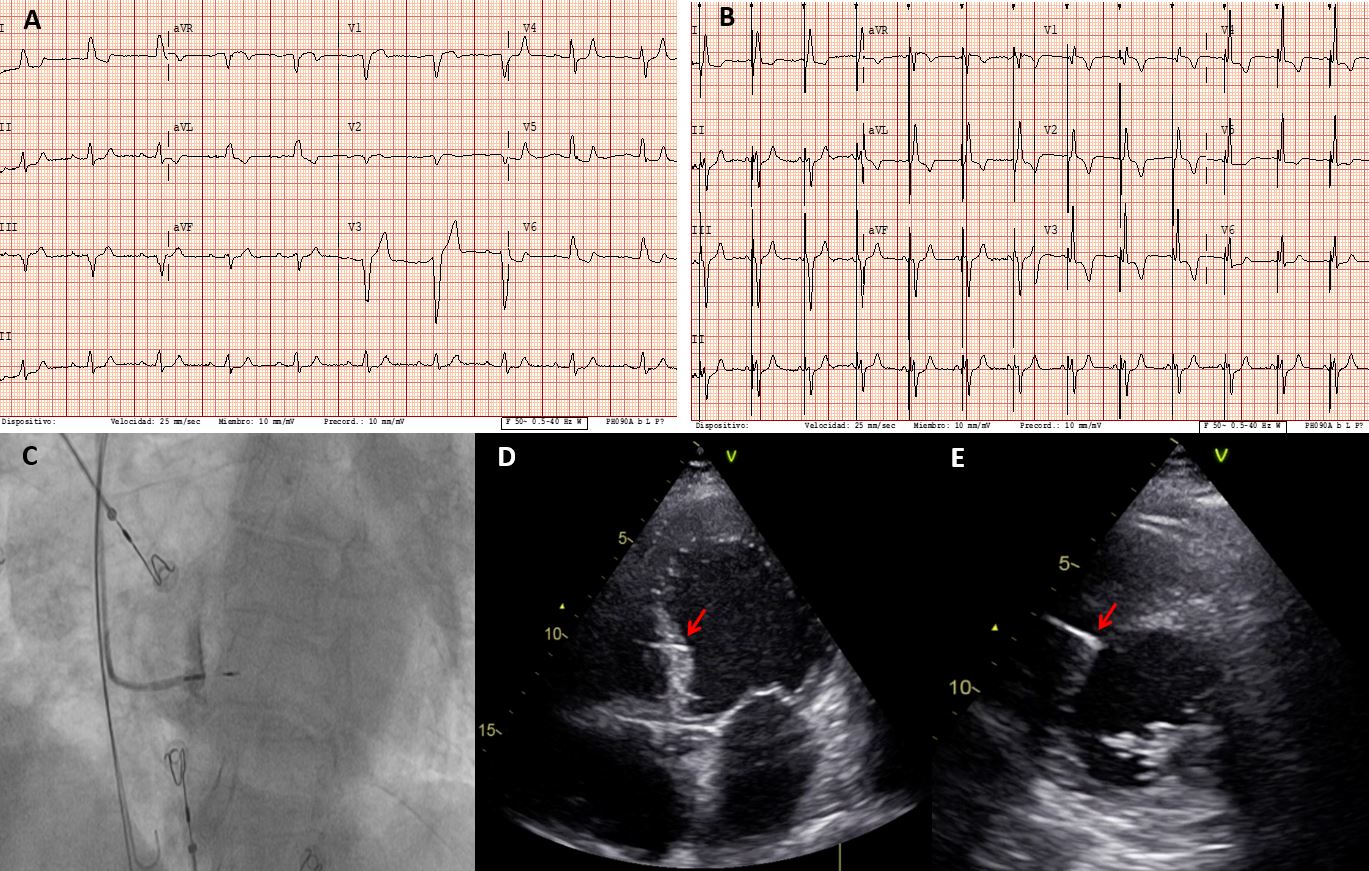
LBBAP was initially described by Huang et al.1 in 2017 as a bail-out strategy after failure of left ventricular (LV) lead placement and His bundle pacing (HBP) during a CRT implant procedure. Since its initial description, the technique has evolved and has been demonstrated to be safe and feasible in a wide range of bradycardia indications.2-4 When compared with HBP in this setting, LBBAP has been shown to have higher rates of implant success, significantly better electrical parameters (pacing threshold and sensed R wave), and lower lead-related complications.5 From a technical point of view, LBBAP appears to be easier than HBP, and the implant technique is reproducible and reliable. Thus, LBBAP has been consolidated as a new conduction system pacing modality together with HBP (Figure 1).
Figure 1: LBBAP in a Patient With LBBB, LVEF of 35%, and Symptomatic Heart Failure
Similar to HBP, LBBAP has also been proposed as a valuable alternative to conventional CRT. The pathophysiological fundamentals of CRT effectiveness are based on the presence of electromechanical dyssynchrony induced by intraventricular conduction disturbances such as LBBB or conventional right ventricular (RV) pacing, which are associated with cardiac adverse remodeling, worsening of systolic and diastolic function, and progressive heart failure.6 CRT obtained via biventricular (BiV) pacing plays a key role in correcting the LBBB-induced dyssynchrony and thus reducing the interventricular and intraventricular dyssynchrony. Multiple randomized clinical trials involving more than 8,000 patients have consistently demonstrated a significant benefit for CRT in terms of morbidity and mortality in patients with heart failure, impaired LV function, and wide QRS.7 Taking into account the pathophysiological fundamentals of CRT, conduction system pacing could be a promising strategy for CRT (Video 1). Although HBP theoretically preserves both RV and LV synchrony and LBBAP would preserve only LV synchrony, different studies have shown that LBBAP can achieve comparable LV activation times and synchrony parameters.8,9 Moreover, myocardial septal capture and retrograde conduction from the left bundle to the right bundle and/or fusion with native right bundle conduction appear to minimize the theoretical loss of RV synchrony during LBBAP.
Video 1
Different observational studies have shown the benefits of HBP CRT in terms of QRS narrowing and improvement in LVEF and functional class.10-13 However, HBP CRT is not infrequently limited by high or unacceptable pacing thresholds or by the inability to correct the bundle branch block. To date, only one randomized study has compared HBP CRT with conventional BiV CRT. The small sample size, high percentage of cross-over, and short-term follow-up preclude any definitive conclusion.14
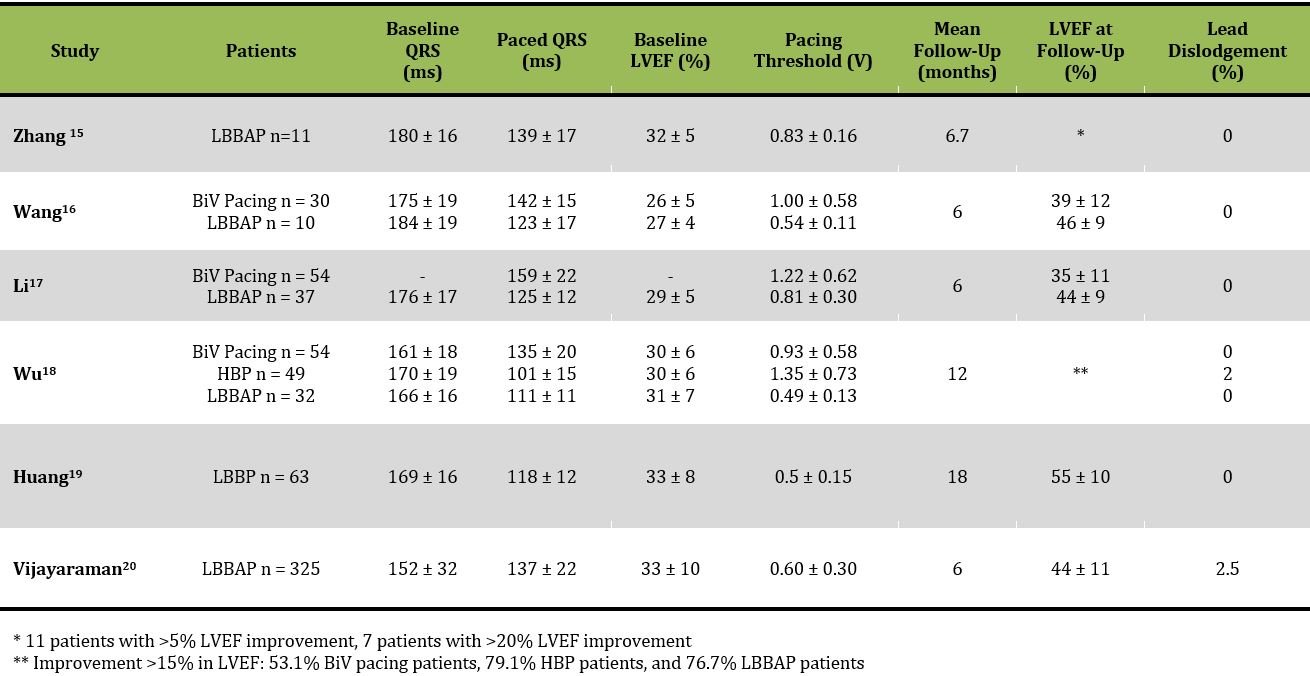
In this scenario, LBBAP has emerged as a new alternative for CRT. Zhang et al.15 reported the first series of 11 patients with CRT indication who underwent LBBAP (Table 1). After LBBAP, QRS duration significantly shortened, as did interventricular mechanical delay and the standard deviation of tissue synchronization imaging of 12 LV segments compared with intrinsic LBBB conduction. Clinical, echocardiographic, and biological parameters (B-type natriuretic peptide) also significantly improved with LBBAP at a mean follow-up of 6.7 months. Two small observational studies have directly compared BiV pacing with LBBAP in patients with CRT indications,16,17 showing significant QRS narrowing and greater LVEF improvement and percentage of echocardiographic response in patients with LBBAP compared with BiV pacing. In the same manner, Wu et al.18 studied 137 consecutive patients referred for CRT who received BiV pacing (n= 54), HBP (n = 49), or LBBAP (n = 32). The paced QRS width significantly improved from baseline in the 3 groups, although QRS narrowing was greater with HBP and LBBAP. LBBAP was associated with better pacing threshold and sensed R wave compared with HBP. At 1-year follow-up, HBP and LBBAP showed significantly higher improvement in LVEF compared with BiV pacing and significantly higher rates of LVEF normalization (74.4%, 70.0%, and 44.9% in HBP, LBBP, and BiV pacing groups; p < 0.001). All groups demonstrated significant improvement in New York Heart Association class, but the improvement was greater for HBP and LBBP groups. Huang et al.19 recently demonstrated 97% success in LBBAP in 63 patients with nonischemic cardiomyopathy and LBBB with improvement in ejection fraction from 33% to 55%.
Table 1: Principal Studies Reporting Data on LBBAP in Patients With CRT Indication
More recently, the results of the International LBBAP Collaborative Study Group have been published.20 This was a retrospective, observational study carried out at 8 institutions in 5 different countries including 325 patients with a CRT indication in which LBBAP was attempted. LBBAP was successfully achieved in 277 patients (85%). Importantly, the electrical parameters obtained at implant were optimal and remained stable during a mean follow-up of 6 ± 5 months. QRS width was also significantly reduced from 152 ± 32 ms to 137 ± 22 ms (p < 0.01). Echocardiographic (≥5% increase in LVEF) and clinical (improvement in New York Heart Association functional class by at least 1 class and no heart failure hospitalization) responses were obtained in 72% and 73% of patients, respectively, with LVEF significantly improving from 33 ± 10% to 44 ± 11% (p < 0.01). Super response (absolute improvement in LVEF of ≥20% or improvement in LVEF to >50% in patients with LVEF ≤35%) was demonstrated in 41 patients (31%) and was more frequent among nonischemic cardiomyopathy patients than ischemic patients (41% vs. 18%; p < 0.01) and tended to be more frequent among patients with LBBB (38% of those with LBBB vs. 24% of those without LBBB; p = 0.09). Of note, echocardiographic response rate was greater among patients with LBBB compared to those without LBBB (87% vs. 67%; p < 0.01).
Considering these preliminary data from observational studies, LBBAP appears as a promising pacing modality for patients with CRT indication. Nevertheless, some important issues remain to be addressed. Long-term follow-up data on safety and efficacy parameters and data from randomized trials comparing LBBAP CRT with conventional BiV pacing are lacking and should be strongly encouraged to definitively elucidate the role of LBBAP in CRT candidates either as an alternative strategy when conventional CRT cannot be achieved or as a first-line therapy in lieu of conventional CRT.
References
- Huang W, Su L, Wu S, et al. A Novel Pacing Strategy With Low and Stable Output: Pacing the Left Bundle Branch Immediately Beyond the Conduction Block. Can J Cardiol 2017;33:1736.e1-1736.e3.
- Vijayaraman P, Subzposh FA, Naperkowski A, et al. Prospective evaluation of feasibility and electrophysiologic and echocardiographic characteristics of left bundle branch area pacing. Heart Rhythm 2019;16:1774-82.
- Li X, Li H, Ma W, et al. Permanent left bundle branch area pacing for atrioventricular block: Feasibility, safety, and acute effect. Heart Rhythm 2019;16:1766-73.
- Padala SK, Master VM, Terricabras M, et al. Initial Experience, Safety, and Feasibility of Left Bundle Branch Area Pacing: A Multicenter Prospective Study. JACC Clin Electrophysiol 2020;6:1773-82.
- Padala SK, Ellenbogen KA. Left bundle branch pacing is the best approach to physiological pacing. Heart Rhythm O2 2020;1:59-67.
- Balla C, Cappato R. When to choose cardiac resynchronization therapy in chronic heart failure: type and duration of the conduction delay. Eur Heart J Suppl 2019;21:B31-B35.
- Cleland JG, Abraham WT, Linde C, et al. An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J 2013;34:3547-56.
- Hou X, Qian Z, Wang Y, et al. Feasibility and cardiac synchrony of permanent left bundle branch pacing through the interventricular septum. Europace 2019;21:1694-702.
- Strocchi M, Lee AWC, Neic A, et al. His-bundle and left bundle pacing with optimized atrioventricular delay achieve superior electrical synchrony over endocardial and epicardial pacing in left bundle branch block patients. Heart Rhythm 2020;17:1922-9.
- Sharma PS, Dandamudi G, Herweg B, et al. Permanent His-bundle pacing as an alternative to biventricular pacing for cardiac resynchronization therapy: A multicenter experience. Heart Rhythm 2018;15:413-20.
- Huang W, Su L, Wu S, et al. Long-term outcomes of His bundle pacing in patients with heart failure with left bundle branch block. Heart 2019;105:137-43.
- Moriña-Vázquez P, Moraleda-Salas MT, Manovel-Sánchez AJ, et al. Early improvement of left ventricular ejection fraction by cardiac resynchronization through His bundle pacing in patients with heart failure. Europace 2020;22:125-32.
- Arnold AD, Shun-Shin MJ, Keene D, et al. His Resynchronization Versus Biventricular Pacing in Patients With Heart Failure and Left Bundle Branch Block. J Am Coll Cardiol 2018;72:3112-22.
- Upadhyay GA, Vijayaraman P, Nayak HM, et al. His Corrective Pacing or Biventricular Pacing for Cardiac Resynchronization in Heart Failure. J Am Coll Cardiol 2019;74:157-9.
- Zhang W, Huang J, Qi Y, et al. Cardiac resynchronization therapy by left bundle branch area pacing in patients with heart failure and left bundle branch block. Heart Rhythm 2019;16:1783-90.
- Wang Y, Gu K, Qian Z, et al. The efficacy of left bundle branch area pacing compared with biventricular pacing in patients with heart failure: A matched case-control study. J Cardiovasc Electrophysiol 2020;31:2068-77.
- Li X, Qiu C, Xie R, et al. Left bundle branch area pacing delivery of cardiac resynchronization therapy and comparison with biventricular pacing. ESC Heart Fail 2020;7:1711-22.
- Wu S, Su L, Vijayaraman P, et al. Left Bundle Branch Pacing for Cardiac Resynchronization Therapy: Nonrandomized On-Treatment Comparison With His Bundle Pacing and Biventricular Pacing. Can J Cardiol 2020;May 7:[Epub ahead of print].
- Huang W, Wu S, Vijayaraman P, et al. Cardiac Resynchronization Therapy in Patients With Nonischemic Cardiomyopathy Using Left Bundle Branch Pacing. JACC Clin Electrophysiol 2020;6:849-58.
- Vijayaraman P, Ponnusamy SS, Cano Ó, et al. Left Bundle Branch Area Pacing for Cardiac Resynchronization Therapy: Results From the International LBBAP Collaborative Study Group. JACC Clin Electrophysiol 2020;Oct 28:[Epub ahead of print].
Clinical Topics: Arrhythmias and Clinical EP, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Echocardiography/Ultrasound
Keywords: Arrhythmias, Cardiac, Natriuretic Peptide, Brain, Bundle-Branch Block, Bundle of His, Bradycardia, Stroke Volume, Stroke Volume, Retrospective Studies, Follow-Up Studies, Cardiac Resynchronization Therapy, Heart Failure, Heart Ventricles, Echocardiography, Electrocardiography, Cardiomyopathies, Morbidity, Hospitalization, Reference Standards
< Back to Listings