Feature | Management of the Hospitalized COVID-19 Patient With Acute Cardiomyopathy or Heart Failure
- Cardiovascular involvement is common in patients with severe COVID-19 disease.
- Cardiomyopathy with SARS-CoV-2 may result from myocarditis, profound systemic inflammation, and/or microvascular dysfunction.
- Evidence of cardiac involvement is associated with worse prognosis in COVID-19.
- Cardiac diagnostic imaging or laboratory testing may be useful in certain patients, but risk vs. benefit and whether additional testing will result in change in management should be considered.
- Background guideline-directed therapy is important to be continued in ambulatory patients who are hemodynamically stable and do not have contraindications.
- Experimental strategies including antiviral, anti-inflammatory, convalescent sera are being considered as part of research protocols or compassionate use for COVID-19 infection with or without cardiac involvement.
- Those with underlying cardiovascular disease are particularly susceptible to cardiovascular complications and mortality with COVID-19.
Cardiomyopathy has been described in patients with severe COVID-19 disease and increasing evidence suggests that cardiovascular involvement portends a high mortality. Viral infection with SARS-CoV-2, the causative agent of COVID-19, has been proposed to impact cardiac function via at least three distinct mechanisms.
First, the later phase of COVID-19 disease is associated with a profound systemic inflammatory response. The cytokines released during this phase have the potential to trigger cardiomyocyte dysfunction and cardiac depression.
This phenomenon has been well described in other inflammatory conditions such as sepsis, where TNFα and IL-1β/β directly suppress cardiomyocyte contractility.1
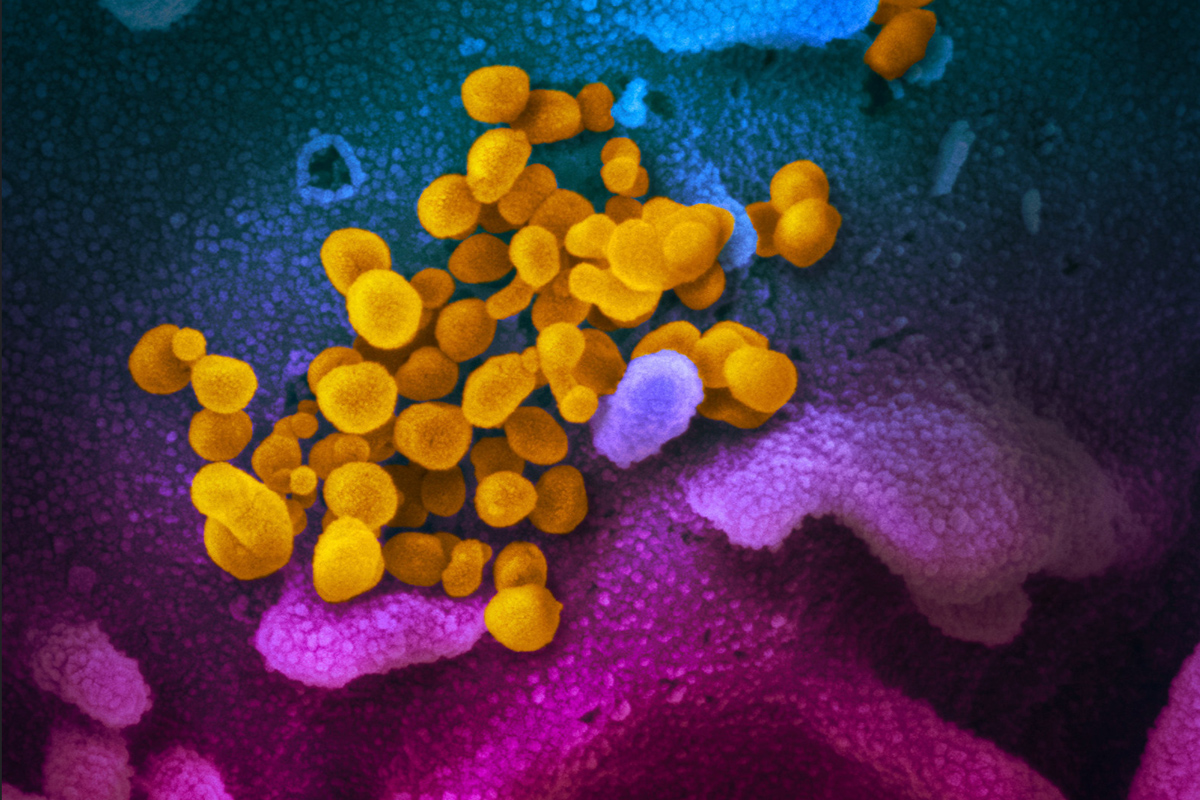 Credit: NIAID-RML
Credit: NIAID-RML
Second, SARS-CoV-2 can directly infect the heart leading to immune cell recruitment and myocarditis. To date, there are few data from patients with COVID-19 to gauge the exact frequency of myocarditis. However, the heart expresses the SARS-CoV-2 receptor ACE2 and MRI-based imaging and ECG findings of myocardial involvement have been reported.2,3
In addition, a study of the related virus SARS-CoV-1, which also uses ACE2 for cell entry, demonstrated the presence of viral RNA in 35% of hearts at autopsy. Interestingly, cardiac tissue from patients with positive viral RNA had an increase in macrophage infiltration, but not a substantial T-cell response.2
Third, infection with SARS-CoV-2 could impact the microvasculature via its effects on ACE2. This could trigger microvascular dysfunction and tissue ischemia leading to ventricular dysfunction and/or arrhythmias.
Ongoing investigation and further autopsy studies will be necessary to determine the proportion of patients with secondary vs. primary cardiac involvement. Those with underlying cardiovascular disease are particularly vulnerable to the cardiac effects of COVID-19-induced inflammation (see below).
Cardiac Involvement With SARS CoV-2 Infection

To date, the amount of granular data about cardiomyopathy in COVID-19 is limited. In an early report of clinical outcomes in 21 patients with severe COVID-19 disease, approximately 30% had evidence of de novo cardiomyopathy.
This was defined as decreased global left ventricular ejection fraction (LVEF) on echocardiogram in association with either elevated cardiac biomarkers, decreased ScVO2, or clinical signs of shock.4
More recently, several larger case series out of China indicate that 20-30% of patients with severe COVID-19 have an elevated troponin.5,6 Echocardiogram results were not reported for most of these of these patients, so it remains unclear what proportion had overt cardiac dysfunction.
However, the presence of cardiogenic or circulatory shock has also been demonstrated in patients with COVID-19 and may account for 7-30% of the mortality resulting from this disease.7
The incidence of cardiac involvement appears to vary from sites around the world and thus it will require detailed reporting from multiple international centers to fully capture this metric.
Prognosis With Cardiac Biomarker Elevation

Although robust characterization of cardiac function is lacking at this time, it is clear that COVID-19 patients with increased troponin and natriuretic peptide levels have a worse prognosis.5,6
This is particularly true in those with underlying cardiovascular disease in whom mortality rates approach 70% in the setting of an elevated troponin.5 By contrast, the mortality in those without cardiovascular disease who have an elevated troponin is closer to 40%.
Patients hospitalized with COVID-19 with a normal troponin have a much better prognosis irrespective of prior cardiovascular disease status (mortality approximately 5-13%).5-7 Ultimately, 50% of patients who die from COVID-19 have elevated serum levels of cardiac biomarkers.7
Mechanisms underlying troponin elevations in COVID-19 patients may include direct viral infection of myocytes, inflammatory cytokine signaling in myocytes, hypotension, and/or ischemia.
It is important to note that elevated troponin levels or evidence of cardiac dysfunction rarely occurs in the absence of severe pulmonary disease, which suggests that isolated myocardial involvement is unlikely to occur with SARS-CoV-2.
Assessment of Cardiomyopathy in COVID-19
There is currently very little data to guide the optimal management of patients with COVID-19 disease who develop cardiomyopathy or mixed/cardiogenic shock. Given the potential for viral spread, decisions about cardiac diagnostic testing and supportive strategies must carefully weigh the risk of exposure with the clinical benefit of the intervention, and whether further testing would make a difference in the management of the patient.
Blood Tests

As discussed earlier, elevated serum troponin and NT pro-BNP identify patients at increased risk of death.5,8 Moreover, these markers signify which patients are at greatest risk of developing cardiomyopathy or cardiogenic shock as these complications are unlikely to occur in the absence of elevated cardiac biomarkers.
In addition, C-reactive protein (CRP), ferritin, D-dimer, IL-6, and LDH are markedly elevated in patients with profound systemic inflammation in response to SARS-CoV-2. These inflammatory biomarkers are also associated with poor prognosis.7,8
ECG
ECG findings with COVID-19 can include diffuse ST-elevations as seen in myopericarditis, nonspecific ST changes, low voltage in the limb leads, and PVCs.9
Although outside the scope of this discussion, patients can also present with STEMI in the setting of COVID-19 and often without evidence of coronary obstruction, perhaps secondary to myocarditis or direct cardiac injury from the virum.
At the present time, the full spectrum of ECG abnormalities has not been well described. It is reasonable to consider ECG in patients with elevated troponin, chest pain, arrhythmia, ST-segment abnormality on telemetry or challenging hemodynamics.
Echocardiography
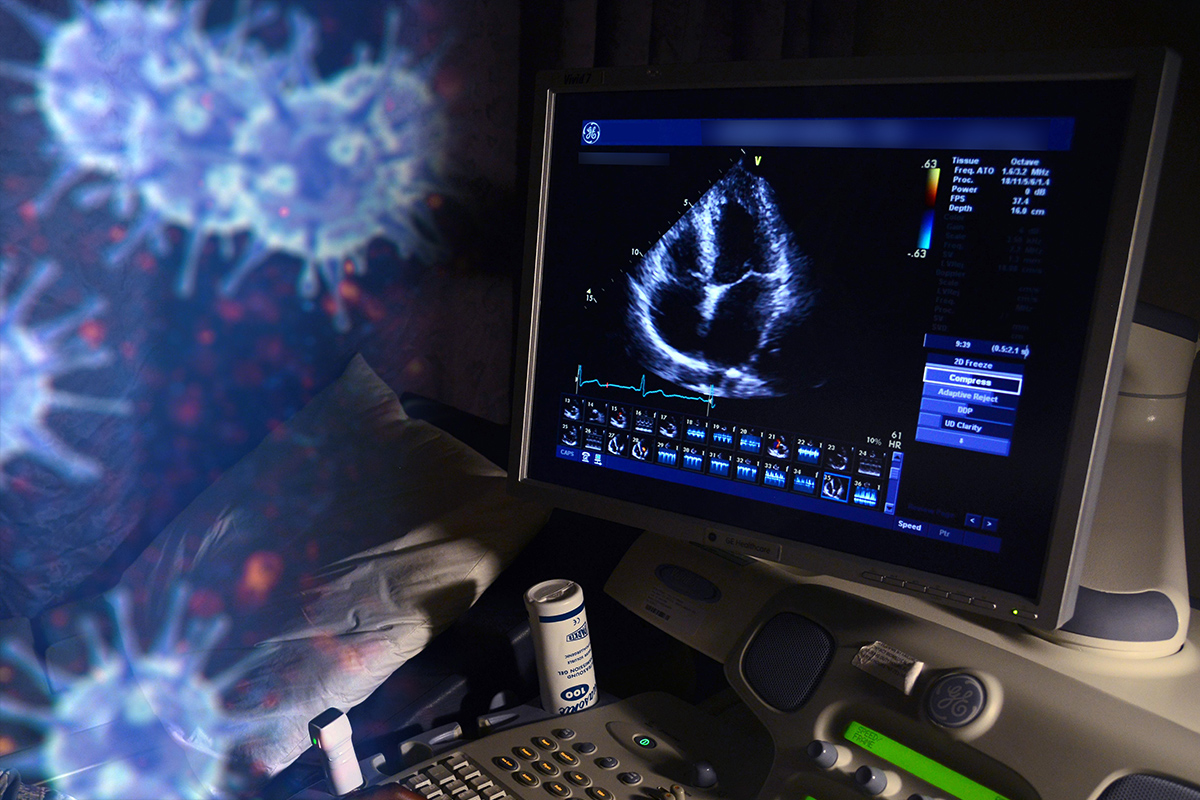
Echocardiography can be useful to assess LV/right ventricular (RV) structure and function, wall motion abnormalities, and to estimate cardiac hemodynamics. However, it is important to minimize sonographer time with COVID-19 positive patients to reduce the risk of spread.
To this end, the decision to obtain an echocardiogram should be made on the basis of patient characteristics, blood test abnormalities, and hemodynamic stability and whether echocardiography information will make a difference in management.
In most cases, a limited study can provide the necessary information for medical decision-making.
Discussing the details of what views are needed with the sonographer before they enter a patient room is important to reduce scan time.
Moreover, the use of point-of-care ultrasound (POCUS) can provide useful information about cardiac function while limiting the number of people that are exposed to an infected patient.
Echocardiography, beyond POCUS, may need to be largely reserved for the subset of patients who require further information beyond what can be provided by POCUS. The presence of reduced LV function and/or myocardial edema could influence the use of inotropic agents, mechanical support or help risk stratify patients for more aggressive anti-inflammatory therapies.
At present, there is minimal role for transesophageal echocardiography and MRI, both of which pose significant risk of aerosolization to the imaging team.
Pulmonary Artery Catheter Assessment

Pulmonary artery catheters (PAC) provide information about hemodynamic status and cardiac filling pressures. Although these data may be useful to direct inotropic and mechanical support in cardiogenic shock, the potential risk of exposure to providers during COVID-19 limits the routine utility of this approach.
Although PACs should not be employed for hemodynamic assessment in all patients with shock, they may have a role in select cases where a patient is responding poorly to empiric vasopressor/inotropic therapy and mechanical support/extracorporeal membrane oxygenation (ECMO) is being contemplated.
In this scenario, careful evaluation of the hemodynamics could instruct the choice of venovenous (VV) vs. venoarterial (VA) ECMO configurations (see below).
It has also been suggested that PAC monitoring might be useful in the management of patients with a history of underlying cardiomyopathy who have a "mixed" cardiogenic-inflammatory shock picture in the context of COVID-19 disease.9
Rather than a PAC, hemodynamic monitoring in most patients can consist of mean arterial pressure (MAP) measurements via an arterial line, central venous pressure (CVP) assessments from a central venous catheter, and monitoring of central mixed venous oxygen saturation (SvO2) saturation.
Endomyocardial Biopsy
Though endomyocardial biopsy can be helpful in the diagnosis of myocarditis, there is currently no evidence to support the use of this procedure in COVID-19, especially if the information would not change management.
In the rare patient with suspicion for myocarditis (such as patients with echo findings of normal LV size, increased wall thickness, and depressed LVEF or cardiac MRI suggestive of myocarditis) in whom the decision to employ aggressive anti-inflammatory or other investigational therapies requires biopsy evidence of myocarditis, this approach could be considered.
Further research will be necessary to determine whether this approach has merit.
Clinical Pearls For Management of Suspected Myocarditis With COVID-19
- In patients hospitalized with COVID-19 cardiac biomarkers should be checked on admission and in follow-up approximately 24-48 hours later.
- Myocarditis or inflammatory cardiac dysfunction should be considered in patients with COVID-19 who have elevated cardiac biomarkers and worsening hemodynamics or arrhythmias.
- ECG should be employed to screen for evidence of ST-T wave changes.
- Maintain a low threshold for POCUS in patients with the above clinical features.
- If evidence of cardiac dysfunction, consider select view for transthoracic echocardiography (TTE) to define LV/RV size and function, wall motion abnormalities, and/or pericardial effusion.
- Stable patients with suspected cardiovascular involvement should continue on guideline-directed medical therapy for heart failure.
- In patients with refractory shock, consider PAC to help guide the use of inotropes, vasopressors or mechanical support.
- Endomyocardial biopsy may have a role in select patients being considered for clinical trials of anti-inflammatory therapy.
Management of Cardiomyopathy in COVID-19
Medical Supportive Care
The mainstay of managing patients with severe COVID-19 disease who have cardiac involvement is supportive care. There is currently no evidence to direct the management of these patients differently than any other inflammatory or "mixed" shock state.
Some general principles include:
- Avoid overaggressive fluid resuscitation given challenges with oxygenation (target CVP 6-8 mm Hg). Higher preload (CVPs 12-15) may also be desirable when significant RV dysfunction and/or high positive end-expiratory pressure (PEEP) states are present. The effective CVP can be calculated by measured CVP – PEEP.
- Target a MAP of 60-65 mm Hg and preferentially start with norepinephrine infusion for hypotension.
- Consider dobutamine in the setting of worsening hypotension with cardiac dysfunction.
- Epinephrine and vasopressin should be considered for refractory hypotension.
- Consideration can be given to using Angiotensin II for refractory vasoplegia.
Mechanical Support/ECMO

There are several factors that must be considered prior to placing a patient with COVID-19 on ECMO support. ECMO is a limited resource and should be reserved for those with the greatest chance of recovery. Therefore, ECMO should not be considered in futility.
The majority of patients being considered for ECMO with COVID-19 disease will have refractory hypoxemia and respiratory acidosis despite advanced ventilator management. In these patients, VV ECMO via internal jugular vein access is most appropriate.
However, in patients with significant cardiomyopathy and cardiogenic shock, a VA ECMO configuration might be necessary.
As discussed above, the use of hemodynamic surrogates and echocardiogram findings can help direct this decision. To this end, VA ECMO has been used to successfully support a patient with COVID-19 who had combined respiratory failure and cardiomyopathy.9
As the majority of patients with circulatory failure also have profound hypoxia, the utility of other cardiac support devices such as intra-aortic balloon pump, TandemHeart or Impella is limited.
To date, ECMO has only been used in a small number of patients with COVID-19 and can be required for several days to several weeks for circulatory support. Additional data regarding patient outcomes following ECMO support will be necessary to shape recommendations for this approach.
Anti-viral/Anti-inflammatory Therapies

Cardiomyopathy in COVID-19 generally appears during the hyper-inflammatory phase of the illness and may be driven, directly or indirectly, by the host immune response to the virus.
Treatment strategies including hydroxychloroquine and azithromycin, anti-inflammatory therapies such as intravenous immune globulin (IVIG), tocilizumab, anakinra, IV steroids and antiviral treatment strategies such as remdesivir, lopinavir and ritonavir have been used or considered in patients with COVID-19.
Given the high mortality in those with cardiomyopathy it is reasonable to consider these options in patients who require ICU care or who decline despite supportive care.
Further research into the cardiovascular and clinical outcomes with these treatments will be necessary to guide recommendations. More detailed discussion of these treatments has been reviewed elsewhere recently.8,11
Summary
Cardiovascular involvement is common with COVID-19 disease and identifies patients at increased risk of death. The precise prevalence and etiology of cardiomyopathy in COVID-19 are not known, but likely results from inflammatory cytokine signaling, myocarditis, and/or microvasculature dysfunction.
To reduce the risk of viral spread, cardiac diagnostic testing should only be performed when the results will directly and immediately change management. Supportive care with vasopressors, inotropes, and possibly ECMO are the mainstays of management.
Ongoing research into the pathogenesis of cardiomyopathy with COVID-19 is warranted and may help identify the optimal approach to assess and manage this particularly high-risk subset of patients.
Another important area of research will be to determine whether there are long-term cardiac sequelae in patients who develop cardiomyopathy with COVID-19 and survive.
References
- Torre-Amione G, Kapadia S, Lee J, et al. Tumor necrosis factor-alpha and tumor necrosis factor receptors in the failing human heart. Circulation 1996;93:704-11.
- Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest 2009;39:618-25.
- Inciardi RM, Lupi L, Zaccone G, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;March 27:[Epub ahead of print].
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA 2020;March 19:[Epub ahead of print].
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;March 27:[Epub ahead of print].
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;March 25:[Epub ahead of print].
- Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 2020;March 3;1-3.
- Akhmerov A, Marban E. COVID-19 and the heart. Circ Res 2020;April 7:[Epub ahead of print].
- Fried JA, Ramasubbu K, Bhatt R, et al. The variety of cardiovascular presentations of COVID-19. Circulation 2020;April 3:[Epub ahead of print].
- Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med 2020;March 11:[Epub ahead of print].
- Li H, Zhou Y, Zhang M, Wang H, Zhao Q, Liu J. Updated approaches against SARS-CoV-2. Antimicrob Agents Chemother 2020;March 23:[Epub ahead of print].
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Stable Ischemic Heart Disease, Valvular Heart Disease, Vascular Medicine, Anticoagulation Management and ACS, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Cardiac Surgery and VHD, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, Acute Heart Failure, Pulmonary Hypertension, Interventions and ACS, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Hypertension, Sleep Apnea, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging, Chronic Angina
Keywords: Acute Coronary Syndrome, Anticoagulants, Arrhythmias, Cardiac, Cardiac Surgical Procedures, Metabolic Syndrome, Angina, Stable, Heart Defects, Congenital, Dyslipidemias, Geriatrics, Heart Failure, Angiography, Diagnostic Imaging, Pericarditis, Secondary Prevention, Hypertension, Pulmonary, Sleep Apnea Syndromes, Sports, Angina, Stable, Exercise Test, Heart Valve Diseases, Aneurysm
< Back to Listings

