Feature | ESC Congress 2018: Our Editors’ Picks

What have we learned from ESC Congress 2018? Among the Hot Line trials, clinical trial updates and late breaking science, there are new findings regarding aspirin, rivaroxaban, lorcaserin and much more. Here’s a roundup of results most likely to influence clinical practice selected by Cardiology’s editors-in-chief.
ASCEND, ARRIVE, COMMANDER HF

The benefit of aspirin in preventing vascular events in patients with diabetes was counterbalanced by major bleeding events in the ASCEND trial. “Even though we showed clearly that aspirin reduces the risk of vascular events, including heart attacks, strokes, and mini-strokes, it also increased the risk of major bleeds, mainly from the gastrointestinal (GI) tract, so overall there was no clear benefit. It had been suggested that low-dose aspirin might protect against cancer, but we saw no reduction in any cancers; we are continuing to follow the participants to see whether any benefits appear later,” said ASCEND principal investigator Jane Armitage.
Using a 2x2 factorial design, ASCEND randomized 15,480 patients aged 40 years and older with diabetes but no history of cardiovascular disease to enteric-coated aspirin 100 mg daily or placebo and to supplementation with Omega-3 fish oil supplements or placebo. During an average 7.4 years of follow-up, the primary efficacy endpoint of first serious vascular event (nonfatal myocardial infarction [MI], nonfatal stroke or cardiovascular death) occurred in 8.5 and 9.6 percent of the aspirin and placebo groups, respectively.
This translates to 11 of every 1,000 participants avoiding a serious vascular event from aspirin, and a 12 percent proportional reduction in risk of serious vascular events. A first major bleed requiring hospitalization or that was fatal occurred in 4.1 and 3.2 percent of the aspirin and placebo groups; meaning nine of every 1,000 participants suffered a first major bleed due to aspirin. The findings were consistent even among participants at the highest cardiovascular risks. No group was identified in whom the benefit of aspirin clearly outweighed the risk.
“Our large, long-term randomised trial shows that fish oil supplements do not reduce the risk of cardiovascular events in patients with diabetes. There is no justification for recommending fish oil supplements to protect against cardiovascular events,” said Louise Bowman, MD. In ASCEND, a first serious vascular event occurred in 8.9 and 9.2 percent of the supplement and placebo groups, respectively. “This is a disappointing finding, but it is in line with previous randomized trials in other types of patient at increased risk of cardiovascular events which also showed no benefit of fish oil supplements,” added Bowman.
The other aspirin study, ARRIVE, showed in a low-risk primary prevention population there was no reduction in the composite primary endpoint, while there was a reduction in first MI, but at the price of a doubling in the risk of GI bleeding. Conducted in seven countries, 12,546 patients with a 10-year risk between 10-20 percent were randomized to 100 mg aspirin or placebo daily.
The primary endpoint – time to first occurrence of cardiovascular death, MI, unstable angina, stroke or transient ischemic attack (TIA) – occurred in 269 and 281 patients in the aspirin and placebo groups, respectively, while GI events occurred in 0.97 and 0.46 percent, respectively.
A lower but nonsignificant risk of a first MI was noted in the aspirin group vs. placebo group. “The ARRIVE data must be interpreted in the context of other studies, which have tended to demonstrate a reduction primarily in MI, but less of an effect on total stroke (including both ischemic and hemorrhagic stroke),” said the study investigators. “The overall decision to use aspirin should be based on individual patient-physician discussion.”
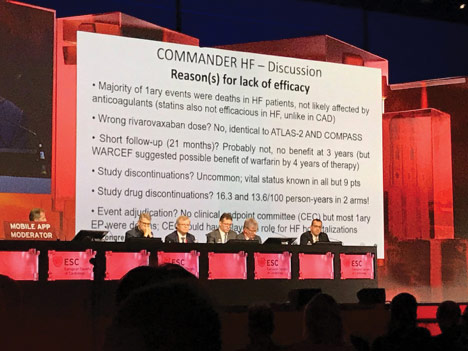
From COMMANDER HF, in patients with coronary artery disease (CAD), worsening heart failure (HF) but no atrial fibrillation (AFib), comes the finding that low-dose (2.5 mg twice daily) rivaroxaban on top of guideline-based therapy did not reduce all-cause mortality, MI or stroke. Similarly, rivaroxaban compared with placebo, did not reduce the risk of cardiovascular death or hospitalization for HF.
During a median follow-up of 21.1 months, the primary endpoint occurred in 25.0 percent of 2,507 patients assigned to rivaroxaban vs. 26.2 percent of 2,515 on placebo. Researchers noted no differences between groups in all-cause mortality or nonfatal MI. However, there was a significantly lower rate of nonfatal stroke with rivaroxaban vs. placebo.
The primary safety outcome occurred in 0.7 and 0.9 percent of the rivaroxaban and placebo groups, respectively. The risk of major bleeding was significantly higher with rivaroxaban vs. placebo. Serious adverse events were reported in 19.2 percent of rivaroxaban and 18.0 percent of placebo patients. More patients taking rivaroxaban than placebo permanently discontinued study medication (7.1 vs. 5.8 percent).
“The most likely reason rivaroxaban failed to improve the primary efficacy outcome is that thrombin-mediated events are not the major driver of cardiovascular events in patients with recent HF hospitalisation,” said study author Faiez Zannad, MD, PhD. “Whether a higher dose of rivaroxaban could have led to a more favourable result is unknown.”
MARINER, COMPASS, GARFIELD-AF
Another trial with rivaroxaban, called MARINER, failed to show any benefit in reducing the primary outcome of risk of symptomatic venous thromboembolism (VTE) or death from VTE when given for 45 days following hospital discharge to patients at increased risk for VTE. The primary outcome occurred in 0.83 percent of rivaroxaban (10 mg once daily) patients and 1.10 percent of placebo patients. There were fewer symptomatic VTE events with rivaroxaban than placebo. The rate of major bleeding was low in both groups: 0.28 and 0.15 percent with rivaroxaban and placebo, respectively.
The investigators stated “the usefulness of extended thromboprophylaxis remains uncertain.” They suggest that “future studies should more accurately identify deaths caused by thrombotic mechanisms and focus on the patients who are at highest risk and who may benefit from anticoagulant prophylaxis.”
ESC Video Highlights
Is CAD an independent risk factor for thromboembolic events, including ischemic stroke, in patients with AFib? This is the finding from a study whose investigators suggest that “CAD should be considered as a potential additional risk factor in the risk scores used for stratification of AFib patients.”
Simultaneously published in the Journal of the American College of Cardiology, the study by Steensig and colleagues examined the association between CAD and stroke in 12,690 AFib patients (≥18 years) undergoing coronary angiography between 2004-2012 in Western Denmark; 59.4 percent had CAD and 40.6 percent did not. The rate of the primary composite outcome of ischemic stroke, TIA and thromboembolism was 2.62 per 100 person-years for patients with CAD and 1.61 per 100 person-years for patients without CAD. Researchers noted the impact of presence of CAD remained significant after adjustment and suggested a 29 percent increased risk of the primary outcome.
Intriguing results from the COMPASS trial suggest that GI and genitourinary (GU) bleeding are powerful predictors of new cancer diagnosis in patients with vascular disease. Furthermore, increased GI bleeding with rivaroxaban appears to unmask cancer even earlier. “The occurrence of GI or GU bleeding in patients receiving antithrombotic drugs should stimulate a search for cancer in the same organ system,” researchers said.
COMPASS randomized 27,395 patients with stable CAD or peripheral artery disease (PAD) to rivaroxaban (2.5 mg bid) plus aspirin, rivaroxaban (5 mg bid) only, or aspirin (100 mg od) only. A total of 1,082 new cancers were diagnosed during the trial, with 23.8 percent diagnosed after bleeding. Of the 307 new cases of GI cancer and 138 new GU cancers, 22.8 and 44.9 percent were diagnosed post bleeding, respectively. Most new GI and GU cancers were diagnosed within six months of a bleed (77.1 and 88.7 percent, respectively).
“More than one in five new diagnoses of cancer are preceded by bleeding,” researchers noted. Within the first year, patients taking rivaroxaban plus aspirin, as well as those taking rivaroxaban alone, had a greater frequency of new GI cancer in the first year (0.6 percent) vs. those taking aspirin (0.4 percent). The investigators also suggest that extended follow-up of COMPASS participants may help show whether earlier identification of cancer after bleeding improves cancer outcomes.
Findings from the GARFIELD-AF registry suggest combined oral anticoagulant (OAC) and antiplatelet therapy is associated with worse outcomes than OAC alone in newly diagnosed AFib patients, especially those without a clear indication for antiplatelet therapy. Data from 25,815 patients with newly diagnosed AFib from 1,317 sites in 35 countries were analyzed. Of these patients, 3,133 were prescribed OAC plus antiplatelet therapy and 22,682 were prescribed OAC alone. Patients were followed for at least 12 months.
The patients receiving OAC plus antiplatelet therapy had a higher prevalence of CAD, acute coronary syndrome and stroke; however, 56 percent did not have CAD or PAD. Patients receiving combined treatment, vs. OAC alone, had an increased risk of major bleeding, all-cause death and stroke. In patients without an indication for antiplatelet therapy, vs. those with an indication, combined treatment was independently associated with increased risk of all-cause death and stroke (hazard ratio, 1.65). However, combined treatment was not harmful in those with an indication.
“These findings challenge the use of combined oral anticoagulant and antiplatelet therapy in patients with AFib, especially those without an indication for antiplatelet therapy,” said Keith A. A. Fox, MB, CHB, FACC, principal investigator. However, Fox noted the findings only apply to full-dose anticoagulation and said AFib patients without CAD or other forms of atherosclerosis who are taking both medications should consult their physicians.
ASCOT Legacy, CAMELLIA-TIMI 61, PURE

The ASCOT Legacy study is “to our knowledge, the first to report that both blood pressure-lowering and lipid-lowering treatments confer such long-term benefits,” said the study investigators. Benefit was shown out to 16 years. “Furthermore, our findings from the non–lipid-lowering arm of the trial, a subgroup at higher cardiovascular risk at baseline, showed that these patients also receive significant long-term benefits from blood pressure-lowering therapies.”
As part of the ASCOT study, all 8,580 UK-based patients with hypertension were randomized to receive either amlodipine-based (n=4,305) or atenolol-based (n=4,275) blood pressure-lowering treatment. Of these patients, those with total cholesterol ≤250 mg/dL and no previous lipid-lowering treatment were further randomized to atorvastatin (n=2,317) or placebo (n=2,288). At 16 years, 1,640 patients assigned to atenolol-based treatment and 1,642 patients assigned to amlodipine-based treatment had died, while 865 of patients also assigned atorvastatin and 903 patients assigned placebo also died.
Researchers noted that among patients receiving blood pressure-lowering treatment, there was no overall difference in all-cause mortality. However, there were significantly fewer stroke deaths in the amlodipine-based treatment group compared with the atenolol group. There were also fewer cardiovascular deaths in patients in the amlodipine group who were not also receiving lipid-lowering treatment. In those receiving lipid-lowering treatment, there were significantly fewer cardiovascular deaths among patients taking a statin vs. those taking placebo.
A related editorial comment in The Lancet, where the results were simultaneously published, noted “the findings of the ASCOT Legacy study have important implications for future long-term follow-up studies of clinical trial participants,” but the current inability to capture nonfatal cardiovascular disease outcomes of participants makes it difficult “to accurately predict how different treatments will affect specific groups.”
The editorial suggests “the need to establish registries to permit long-term assessment of morbidity and mortality in participants involved in randomized controlled trials of interventions for cardiovascular disease.” It also notes that electronic health records can facilitate this process, provided national regulations are established.
A weight loss drug, lorcaserin, did not increase cardiovascular events in the CAMELLIA-TIMI 61 trial. “We have been able to show for the first time that this weight loss drug does what it is intended to do. It helps people lose weight without causing an increase in MACE [major adverse cardiovascular events] in a population at higher risk for heart attacks and strokes,” said Erin Bohula, MD, an investigator with the trial. “One of our hypotheses was that losing weight with this medication might also lead to a cardiovascular benefit but we did not see that.”
CAMELLIA-TIMI 61 enrolled 12,000 adults from 473 centers in eight countries between January 2014 and November 2015. All participants had a minimum BMI of 27 kg/m2 and either established cardiovascular disease (with or without diabetes) or diabetes and at least one cardiovascular risk factor. Participants were randomized to lorcaserin (10 mg twice daily) or placebo and followed for a median of 3.3 years.
The primary safety endpoint of noninferiority for MACE was met by lorcaserin vs. placebo, with MACE occurring in 6.1 and 6.2 percent of the groups, respectively. However, it did not meet the superiority endpoint for the composite of MACE plus hospitalization for unstable angina, HF or any coronary revascularization (11.8 vs. 12.1 percent, respectively).
The average weight loss in the first year was 4.2 kg with lorcaserin and 1.4 kg with placebo. Moreover, a weight loss of at least 5 percent of body weight at one year was achieved by 39 percent of the drug treatment group, but 17 percent of the placebo group. At 3.3 years of follow-up, the between-group differences remained significant. Also of note, the conversion rate from prediabetes to diabetes was lower with lorcaserin than placebo, and the drug led to small improvements in triglycerides, blood glucose, heart rate and blood pressure.
In an editorial comment accompanying the published results in the New England Journal of Medicine, Julie R. Ingelfinger, MD, and Clifford J. Rosen, MD, question whether the drug is an “elixir or liability.” They caution that for now “the drug may be best used on a cautious basis according to the needs of individual patients” given its side effects and the need for more long-term data. Side effects included headache, fatigue, dizziness, diarrhea and nausea and led to twice the number of discontinuations in the lorcaserin than placebo group, even though the total rates of discontinuation in both groups were similar.
What comprises a healthy diet? Results from the PURE study suggest it’s one consisting of higher intakes of fruit, vegetables, nuts, legumes, fish, dairy products and unprocessed meat. But, elements of the findings differ from current diet advice based on previous studies conducted largely in high-income countries.
The investigators derived a dietary quality score based on foods associated with a lower risk of death in participants in the PURE study. More than 218,000 participants in five studies (PURE, ONTARGET, TRANSCEND, INTERHEART, INTERSTROKE) from over 50 countries in five continents were divided into five groups based on the quality of their diet. Researchers then compared the risks of cardiovascular disease and death in those with the highest quality diet with the poorest quality diet. The high-quality diet included three daily servings of a dairy product and 1.4 servings of unprocessed meat.
Over the median 9.1 years of follow-up, there were 6,821 deaths and 5,466 major cardiovascular events (death from cardiovascular causes, nonfatal MI, stroke, HF). Across participants in all five studies, the highest quality diet was associated with lower risks of major cardiovascular events, including stroke, cardiovascular death and noncardiovascular death. Results were consistent across patients with and without cardiovascular disease.
Based on the PURE findings, the researchers suggest people around the world should limit the amount of refined carbohydrates and note that dairy foods and unprocessed meat can be included as part of a healthy diet. “Thinking on what constitutes a high quality diet for a global population needs to be reconsidered,” said Salim Yusuf, DPhil, FACC, senior author. “For example, our results show that dairy products and meat are beneficial for heart health and longevity. This differs from current dietary advice.”
“Studies like this are very interesting and can add to the knowledge base, but should be interpreted with caution, particularly when comparing multiple countries with marked differences in socioeconomic status as well as food preparation differences,” noted Gaurav Sharma, MD, and Andrew Freeman, MD, FACC. They added, “the findings regarding red meat and dairy consumption in the PURE diet score should be taken with reservation. Findings from other randomized and observational studies demonstrating adverse cardiovascular outcomes with increased animal fat consumption should not be displaced just yet – more work is still needed.”
Dialing in on Telemedicine Research

Whether its assessing remote management of HF patients or use of mobile technologies to screen patients with AFib, the ability of telemedicine to improve patient outcomes continues to be a focus of new research.
In the TIM-HF2 trial, the percentage of days lost to unplanned hospital readmissions or all-cause death was 4.88 percent in patients randomized to a structured remote patient management program, vs. 6.64 percent in patients randomized to usual care. A total of 1,571 patients from hospitals and cardiology practices in Germany were randomized and followed for up to 393 days. The number of days lost per year was about 18 in the remote management group and about 24 in the usual care group.
“To the best of our knowledge, this is the first RCT to use a structured remote patient management intervention that was designed to be a true holistic approach for the management of patients with HF, involving cardiologists, general practitioners, nurses, other health-care providers, and the patient,” researchers said. They noted the concept of “a telemedical center with physicians and HF nurses available 24 hours a day, every day, and able to act promptly according to the individual patient risk profile” was a key factor.
The DIGITAL-AF study found AFib can be identified using a smartphone application that employed pulse-plethysmography (PPG) through the phone’s camera. Investigators recruited 12,328 participants via a local newspaper. Participants used their own smartphone to measure their heart rhythm twice daily and when experiencing symptoms over a nine-day period.
In total, 80 percent of participants were identified with sinus rhythm and 1.1 percent with AFib; 17 percent with irregularities not related to AFib and 2 percent without high-quality measurements. In the AFib group, the average age was 62.8 years and 70 percent were men. Most (75 percent) were asymptomatic, 28 percent had persistent AFib (all detected on first PPG measurement) and 72 percent had paroxysmal AFib.
A follow-up questionnaire four months later to assess the impact of the screening was completed by 100 of the 136 patients identified with AFib, of whom 53 percent consulted a medical professional to confirm the diagnosis. Of the 60 patients who had been previously diagnosed with AFib, the screening resulted in 28 percent receiving adjustments to their current care strategy following consultation with their care providers.
“These results indicated a high yield of newly identified AFib patients without utilizing excessive health care resources,” researchers noted. “This novel digital methodology requires future research but already demonstrates its potential as a scalable, reliable and cost-effective screening tool for AFib.”
Two other trials in the telemedicine session – REMOTE-CIED and RM-ALONE – addressed remote monitoring as a promising method for following patients with cardiac implantable electronic devices. And, providing reassurance for patients with devices, a study presented in another late-breaking session showed that security body scanners are safe for patients with pacemakers, ICDs and CRT devices.
“We found no evidence of electromagnetic interference or device malfunction with the full body scanner we tested and can conclude that scanning is safe for patients with implanted cardiac devices,” said Carsten Lennerz, MD, study author. The study mimicked the same electromagnetic fields used in real life, but in a controlled hospital setting. Based on their findings, he suggests there’s little need for specific protocols or restrictions on the use of body scans in people with pacemakers and other implantable devices.
Interventional Cardiology
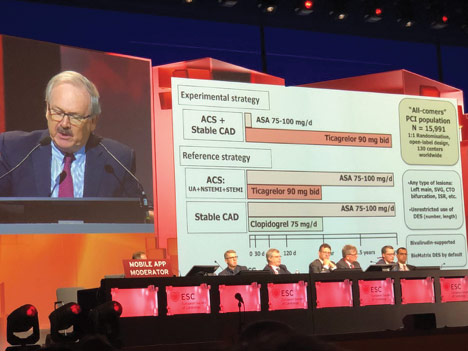
Before we go, CULPRIT-SHOCK showed that culprit-lesion only PCI, vs. multivessel PCI, reduced the risk of death or renal replacement therapy at one year in patients with acute MI and cardiogenic shock. GLOBAL LEADERS showed that while long-term antiplatelet therapy, vs. standard therapy, post DES implantation is safe, it did not reduce death or MI risk. SCOT-Heart showed computed tomographic angiography plus standard care, vs. standard care alone, in patients with stable chest pain may lead to lower rates of death from coronary heart disease or nonfatal MI at five years. Read more about these at ACC.org/ESC2018 and in the September-October issue of Cardiology: Interventions.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Geriatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Stable Ischemic Heart Disease, Vascular Medicine, Anticoagulation Management and ACS, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, Acute Heart Failure, Chronic Heart Failure, Pulmonary Hypertension, Interventions and ACS, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Hypertension, Chronic Angina
Keywords: ACC Publications, Cardiology Magazine, Acute Coronary Syndrome, Anticoagulants, Arrhythmias, Cardiac, Cardiac Surgical Procedures, Metabolic Syndrome, Angina, Stable, Heart Defects, Congenital, Dyslipidemias, Geriatrics, Heart Failure, Heart Failure, Systolic, Hypertension, Pulmonary
< Back to Listings








