The Myriad Cardiovascular Effects of Obesity
Quick Takes
- Obesity is associated with increased risk of coronary artery disease, heart failure, and arrhythmias.
- Lifestyle counseling is integral to promoting improvements in diet and physical activity to reduce the risk of obesity and adverse CVD outcomes.
- Clinicians should make use of a streamlined behavior change framework to aid in the effective delivery of lifestyle counseling within the time constraints of an office visit.
Trends in Obesity Prevalence
The American Heart Association (AHA) scientific statement on obesity highlights its impact on many forms of cardiovascular disease (CVD).1 Rates of overweight, defined as body mass index (BMI) ≥25, and obesity (BMI ≥30) have increased in recent decades; the World Health Organization (WHO) estimates that in 2016, 39% of adults were overweight and 13% of adults had obesity.2 By 2030, one in two United States (US) adults will have obesity and one in four will have severe obesity, with even higher rates among certain sociodemographic subgroups.3 Given its increasing prevalence, obesity threatens to reverse decades of decreases in CVD mortality. Therefore, understanding the role of obesity in CVD development and what can be done about it is of upmost importance.
The reasons behind recent increases in obesity prevalence in the US are complex, with both socioeconomic and cultural factors playing important roles.4 Many of the same factors that contribute to increasing obesity rates are CVD risk factors and put these individuals at disproportionately high risk for adverse outcomes.
Assessment of Adiposity – Beyond BMI
BMI has traditionally been the measure used to assess body fat. While convenient in terms of its ease of calculating, BMI is an imperfect tool. In addition to variations in body composition across sex, age, and race/ethnicity, it does not fully capture abdominal obesity and visceral adiposity, which are strongly associated with CVD.5
Measurement of waist circumference (WC) and WC-to-hip ratio (WHR), which are surrogate markers for abdominal and visceral fat, correlate poorly with BMI; they are independently associated with CVD risk and provide additional prognostic information.1 Direct measurement of visceral adipose tissue (VAT) and ectopic fat (e.g., pericardial, hepatic) stores using computed tomography (CT) or magnetic resonance imaging (MRI) are even stronger predictors of metabolic and CVD risk.5 Elevated WC combined with hypertriglyceridemia is highly predictive of increased VAT, and is a clinically useful phenotypic marker of elevated risk.
Impact of Obesity on CVD Subtypes
The AHA statement summarizes the link between obesity and CVD subtypes.1
1. Coronary artery disease (CAD)
A meta-analysis of nearly one million patients found elevated CAD risk among participants with obesity.6 Central obesity, as evidenced by elevated WC or WHR, has been associated with increased mortality from CAD,7 even among those with a normal BMI.
Hypertension, insulin resistance, and dyslipidemia are mediators of the relationship between obesity and CAD, but obesity-associated inflammation driven by adipocytokines and oxidative stress promote atherogenesis.1 Increased aerobic exercise and adherence to a Mediterranean diet pattern decrease CVD risk.
While lifestyle improvements may lead to weight loss, some studies focusing on interventions to promote weight loss have not shown an associated reduction in risk.8 Conversely, studies of patients undergoing bariatric surgery, in which the amount of weight loss was greater, have shown a significant CAD risk reduction.9 The lack of significant risk reduction with lifestyle interventions may be due to the relatively modest degree of weight loss in these trials, highlighting the potential benefits of complementary strategies for weight loss. Additionally, while promotion of a healthy weight is important, encouraging patients to set goals around diet and physical activity measures have benefits beyond resultant weight loss.10
2. Heart failure (HF)
Overweight and obesity are also well-established risk factors for HF, especially HF with preserved ejection fraction (HFpEF). Obesity and VAT have direct effects on the vasculature that promote systolic and diastolic dysfunction.1 The association of obesity with HF may be partly explained by low cardiorespiratory fitness (CRF), and observational data suggest higher physical activity is associated with reduced HF risk.11 For patients with stable chronic HF, participation in a supervised cardiac rehabilitation program may result in improvement in health-related quality of life.12
3. Arrhythmia
Obesity is linked with increased risk for arrhythmias including atrial fibrillation (AF) and ventricular arrhythmias; for every 5 unit increase in BMI, there is an associated 29% increased risk of AF13 and 16% increased risk of sudden cardiac death.14 Risk of progression from paroxysmal to permanent AF also increases as BMI increases.13
Multiple mechanisms likely account for this, including obesity-associated myocardial remodeling and fibrosis,1 as well as increased epicardial adipose tissue. Weight loss and cardiometabolic risk factor control results in an impressive reduction in AF symptoms and severity.13
Lifestyle Counseling: a Practical Approach for Clinicians and Patients
The AHA's statement highlights the role of weight loss, healthy diet, and physical activity to improve obesity associated outcomes. Primary care-focused interventions that promote a healthy diet and physical activity have beneficial effects on health behaviors in patients with CVD risk factors.15
Ideally, promotion of these tenants of a healthy lifestyle should happen at all clinic visits, starting in a primary care setting before patients develop manifest CVD and should be continued by cardiovascular specialists. However, office visits are often rushed with many important topics to cover. Thus, a streamlined, practical approach for clinicians is needed to more effectively counsel patients.
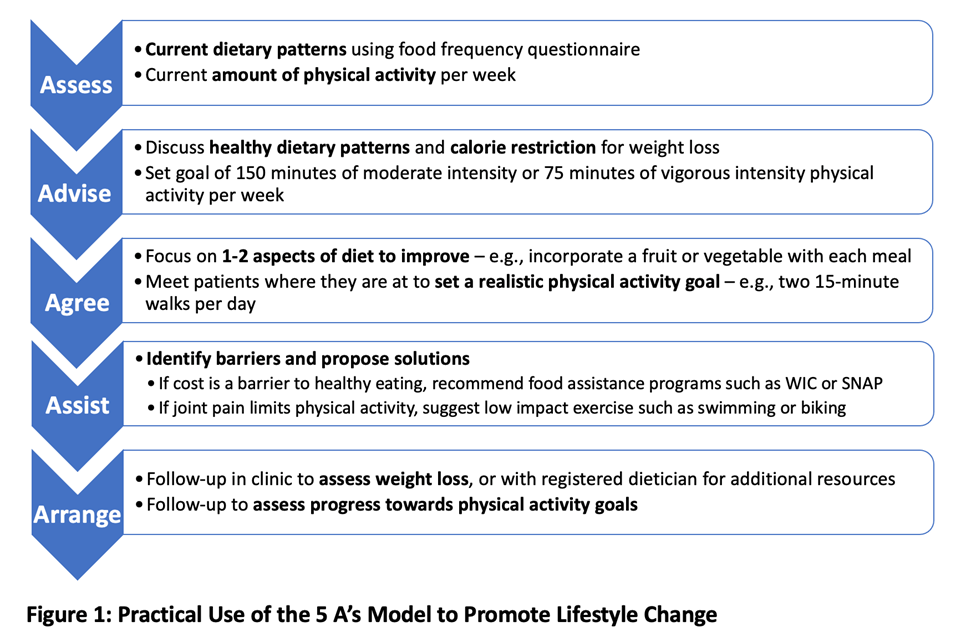
Use of a behavior-change model, such as the "5 A Model" (Assess, Advise, Agree, Assist, and Arrange) supported by US Preventive Services Task Force, can provide a framework for discussion and aid in goal-setting, problem-solving, and following up on goal progress.16 Clinicians delivering this counseling should be familiar with additional resources such as nutritionists, dieticians, food assistance and exercise programs available for their patients and provide referrals as appropriate.
Figure 1
Focusing on one health behavior per visit can help to make the task seem more achievable. Given the benefits of healthy diet and physical activity,10 these tenants would be a good place to start. Guidance should focus on dietary patterns that emphasize vegetables, fruits, legumes, whole grains, and lean protein and minimize intake of refined carbohydrates, sweetened beverages, processed meats, dietary cholesterol and sodium, and avoidance of fad diets.17 For exercise, 150 to 300 minutes of moderate to vigorous physical activity per week is recommended.18
Conclusions
The AHA's recent scientific statement provides a comprehensive overview of the cardiovascular effects of obesity and highlights the role of lifestyle interventions. The obesity epidemic remains a complex issue with socioeconomic and cultural ties. While the global health community should develop policies at the population level, the impact of lifestyle counseling by individual clinicians cannot be overlooked. A streamlined approach to diet and exercise counseling is necessary so that the messages can be effectively delivered to patients within the constraints of a typical office visit.
References
- Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2021;143:e984-e1010.
- Obesity and overweight (World Health Organization website). 2021. Available at https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 06/01/2021.
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med 2019;381:2440–50.
- Bell CN, Kerr J, Young JL. Associations between obesity, obesogenic environments, and structural racism vary by county-level racial composition. Int J Environ Res Public Health 2019;16:861.
- Neeland IJ, Ross R, Despres JP, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 2019;7:715–25.
- Riaz H, Khan MS, Siddiqi TJ, et al. Association between obesity and cardiovascular outcomes: a systematic review and meta-analysis of mendelian randomization studies. JAMA Netw Open 2018;1:e183788.
- Sharma S, Batsis JA, Coutinho T, et al. Normal-weight central obesity and mortality risk in older adults with coronary artery disease. Mayo Clin Proc 2016;91:343–51.
- Kuno T, Tanimoto E, Morita S, Shimada YJ. Effects of bariatric surgery on cardiovascular disease: a concise update of recent advances. Front Cardiovasc Med 2019;6:94.
- Fisher DP, Johnson E, Haneuse S, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. JAMA 2018;320:1570–82.
- Maron DJ, Mancinin GBJ, Hartigan PM, et al. Healthy behavior, risk factor control, and survival in the COURAGE Trial. J Am Coll Cardiol 2018;72:2297–2305.
- Pandey A, Cornwell WK III, Willis B, et al. Body mass index and cardiorespiratory fitness in mid-life and risk of heart failure hospitalization in older age: findings from the Cooper Center Longitudinal Study. JACC Heart Fail 2017;5:367–74.
- Taylor RS, Walker S, Smart NA, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: individual participant meta-analysis. J Am Coll Cardiol 2019;73:1430–43.
- Nalliah CJ, Sanders P, Kottkamp H, Kalman JM. The role of obesity in atrial fibrillation. Eur Heart J 2016;37:1565–72.
- Aune D, Schlesinger S, Norat T, Riboli E. Body mass index, abdominal fatness, and the risk of sudden cardiac death: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol 2018:33;711–22.
- Krist AH, Davidson KW, Mangione CM, et al. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force Recommendation Statement. JAMA 2020;324:2069–75.
- Educational Information for Health Professionals (US Preventive Services Taskforce website). Available at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/tools-and-resources-for-better-preventive-care. Accessed 06/01/2021.
- 2015-2020 Dietary Guidelines for Americans (health.gov). 2015. Available at: https://health.gov/our-work/food-nutrition/previous-dietary-guidelines/2015. Accessed 06/01/2021.
- Physical Activity Guidelines for Americans, 2nd edition (health.gov). 2018. Available at: https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. Accessed 06/01/2021.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Sports and Exercise Cardiology, Atherosclerotic Disease (CAD/PAD), SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Computed Tomography, Magnetic Resonance Imaging, Nuclear Imaging, Diet, Exercise, Hypertension, Stress, Sports and Exercise and Imaging
Keywords: Dyslipidemias, Body Mass Index, Obesity, Abdominal, Intra-Abdominal Fat, Cholesterol, Dietary, Quality of Life, Corticotropin-Releasing Hormone, Adiposity, Waist Circumference, Weight Loss, Cardiovascular Diseases, Adipokines, Obesity, Morbid, Diet, Cardiac Rehabilitation, Insulin Resistance, Metabolic Syndrome, American Heart Association, Heart Failure, Coronary Artery Disease, Atrial Fibrillation, Global Health, Ethnic Groups, Stroke Volume, Exercise, Health Behavior, Bariatric Surgery, Hypertriglyceridemia, Magnetic Resonance Imaging, Hypertension, Biomarkers, Inflammation, Carbohydrates, Atherosclerosis, Death, Sudden, Cardiac, World Health Organization, Ambulatory Care, Oxidative Stress, Fibrosis, Referral and Consultation, Primary Health Care, Outcome Assessment, Health Care, Tomography, X-Ray Computed, Socioeconomic Factors, Exercise Therapy, Risk Reduction Behavior, Tomography, Primary Prevention, Sports
< Back to Listings