For the FITs | Antiplatelet Therapy For High Bleeding Risk Patients Undergoing PCI
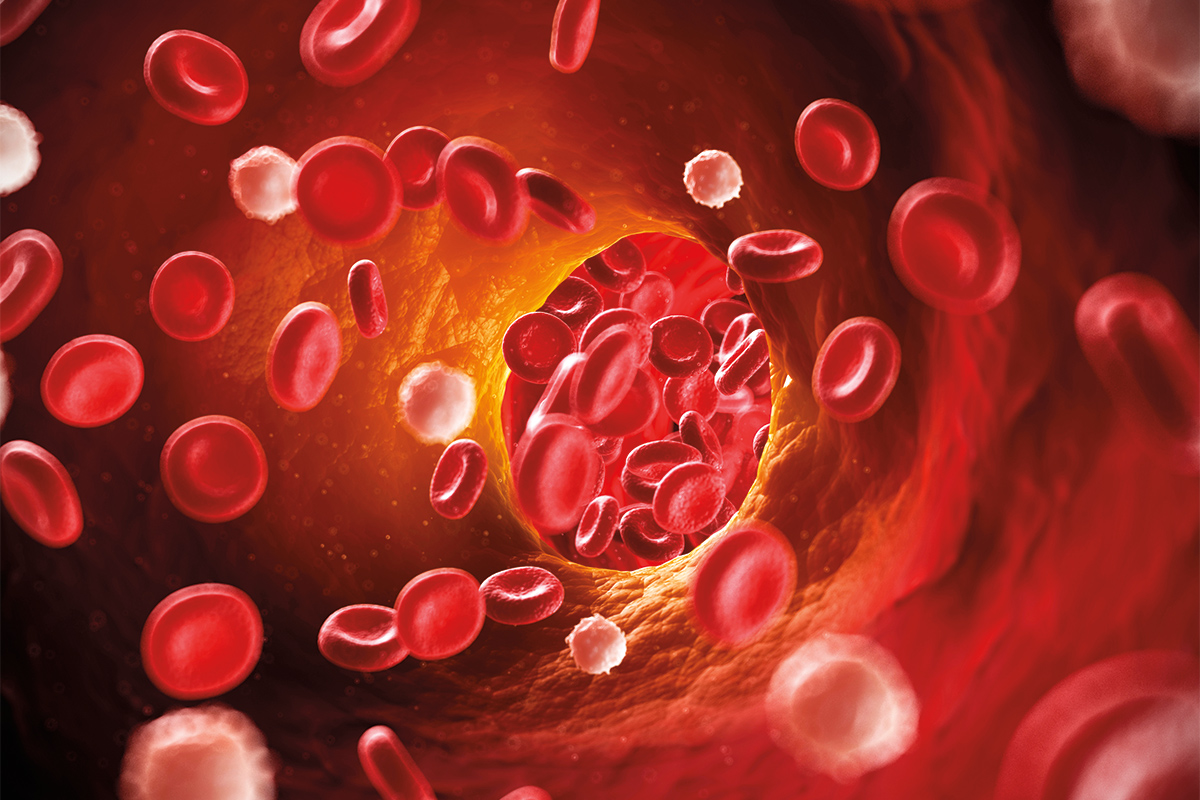
Coronary revascularization with PCI involves the use of balloon angioplasty and intracoronary stenting to improve coronary blood flow. PCI with intracoronary stents requires treatment with dual antiplatelet therapy (DAPT) for a period as short as one month to as long as three years.1,2
DAPT after PCI improves morbidity and mortality by reducing ischemic events but increases bleeding risk, especially for high bleeding risk (HBR) patients. Nearly one-third of patients treated with PCI are considered to be at HBR, but these patients are frequently excluded from stent trials.3
The following is a brief primer on use of antiplatelet therapy in HBR patients undergoing PCI in light of emerging data in this area.
Definition of High Bleeding Risk
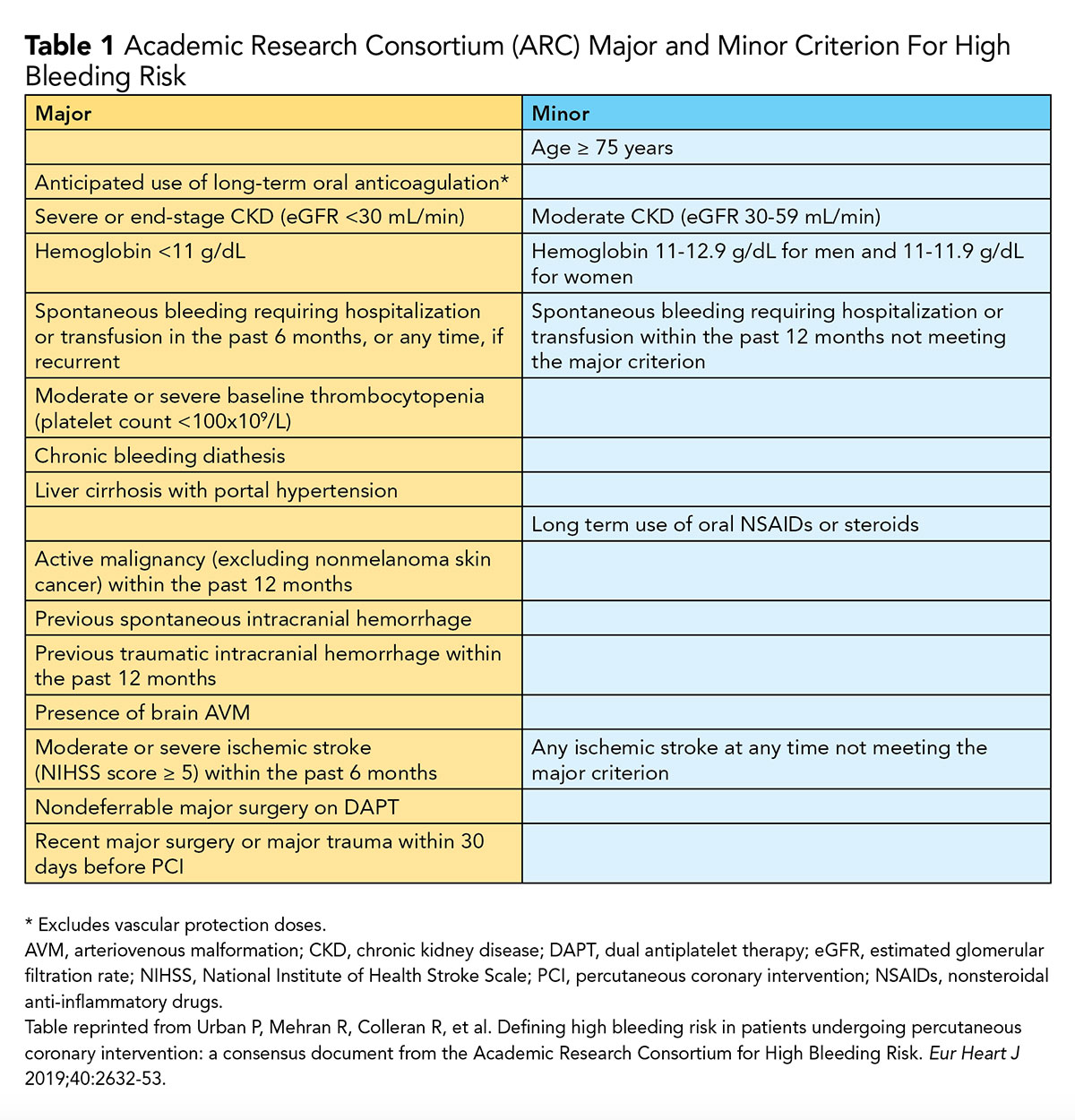
The most commonly used definition of HBR is the one established by the Academic Research Consortium for High Bleeding Risk (ARC-HBR), which specifies 20 clinical criteria (14 major, 6 minor); the presence of at least one major or two minor criteria (risk factors) for major bleeding defines HBR.3
Although this definition is binary, it acknowledges that the bleeding risk is increased further with an increase in the number of major or minor criteria. ARC-HBR clinical criteria that predict major bleeding are summarized in Table 1.
Incidence of Bleeding After PCI
Bleeding and bleeding-related hospitalization are common in patients receiving DAPT after PCI. In studies evaluating bleeding and thrombotic risk in patients treated with DAPT after coronary stenting, clinically relevant bleeding occurred in up to 6.2% of patients and up to 4.8% patients had bleeding-related hospitalization.4,5
The most common source of bleeding is the gastrointestinal tract, with the majority of bleeding occurring within 30 days post discharge. Bleeding while on DAPT after PCI frequently leads to nonadherence to DAPT and any bleeding, particularly major bleeding, after PCI carries a poor prognosis.
Assessing Bleeding Risk
Various risk prediction models for HBR incorporate the risk factors listed in Table 1. However, given the heterogeneity in the variables assessed, bleeding definition used and the risk factors used, there are differences between models when applied to an individual patient.
HAS-BLED (Hypertension, Abnormal renal and liver function, Stroke, Bleeding tendency or predisposition, Labile INRs [for patients taking warfarin], Elderly (age >65 years), Drugs [aspirin, NSAIDs, excess alcohol use]) is the most commonly used bleeding risk score, developed to assess bleeding risk in patients with atrial fibrillation and has not been validated in patients receiving DAPT.
The PRECISE-DAPT score is a five-item risk score developed to predict out-of-hospital bleeding risk during treatment with DAPT.6
The DAPT score was created to predict risk/benefits of extending DAPT treatment beyond 12 months after coronary stenting, but it does not apply to HBR patients because the DAPT study excluded patients on oral anticoagulation and those with GUSTO moderate-to-severe bleeding during initial treatment with DAPT.2
Balancing Bleeding and Ischemic Risk
The risk of stent thrombosis is the highest within the first 30 days after PCI, whereas the risk of bleeding with DAPT remains relatively constant throughout the duration of treatment with DAPT. Thus, the benefits of DAPT are the greatest during the first 30 days after intervention, whereas daily risk of stent thrombosis continues to fall with time after 30 days and is much smaller after six months.
Role of Balloon Angioplasty and Choice of Stent
Due to the high risk of acute vessel closure, plain old balloon angioplasty (POBA) is generally not considered to be as prudent a revascularization strategy as stenting. POBA is usually reserved for rare cases where a stent cannot be delivered or when DAPT cannot be administered for a minimum of 30 days.
PCI with a drug-coated (-eluting) balloon (DCB) offers the potential to avoid long-term DAPT. In Europe, it is approved for treatment of in-stent restenosis and de-novo lesions in small coronary arteries.
However, due to limited data with DCBs to date, coronary DCBs have not been approved in the U.S. and additional studies are necessary before routine use of DCBs in HBR patients can be recommended.
Although there is no strong evidence to suggest the use of a bare-metal stent (BMS) compared with drug-eluting stents (DES) allows for a shorter period of DAPT or improves outcome in HBR patients, previously BMSs were used in an effort to curtail DAPT use to 30 days in these patients. Several recent studies have evaluated the utility of a short duration of DAPT in HBR patients treated with DES.
For example, the ZEUS trial (Zotarolimus-eluting Endeavor sprint stent [ZES] in Uncertain DES candidates) randomly assigned patients with HBR, low restenosis risk and high stent thrombosis risk to BMS or ZES. Patients were treated with DAPT for a mean duration of 32 days followed by aspirin or P2Y12 monotherapy.

Patients treated with ZES had a significantly lower rate of major adverse cardiac events (including death, myocardial infarction [MI], target vessel revascularization [TVR]) at 12-months follow-up (17.5% vs. 22.1%; hazard ratio [HR], 0.76; 95% confidence interval [CI], 0.61-0.95) with the difference primarily driven by lower rates of MI and TVR in patients treated with ZES.7
A prespecified analysis from ZEUS of the 828 patients at HBR also showed that major adverse cardiac event occurred less often with ZES (22.6% vs. 29%; HR, 0.75; 95% CI, 0.57-0.98).
The LEADERS FREE trial demonstrated that a polymer- and carrier-free umirolimus-coated stent was superior in safety and effectiveness to a BMS in patients at HBR who received one month of DAPT.8
Similarly, the SENIOR trial randomized 1,200 patients aged 75 years or older scheduled to undergo PCI to either a bioresorbable polymer DES or similar thin-strut BMS.
Patients were treated with DAPT for six months in cases of acute coronary syndrome and for one month for stable patients. The primary composite endpoint (all-cause mortality, MI, stroke, or ischemia-driven TVR) occurred significantly less often in the DES group (12% vs. 16%; relative risk, 0.71; 95% CI, 0.52-0.94).9
As summarized in Table 2, several recent randomized and registry-based studies have demonstrated safety and efficacy of short duration DAPT in HBR patients treated with PCI. There are also several ongoing studies evaluating these patients.
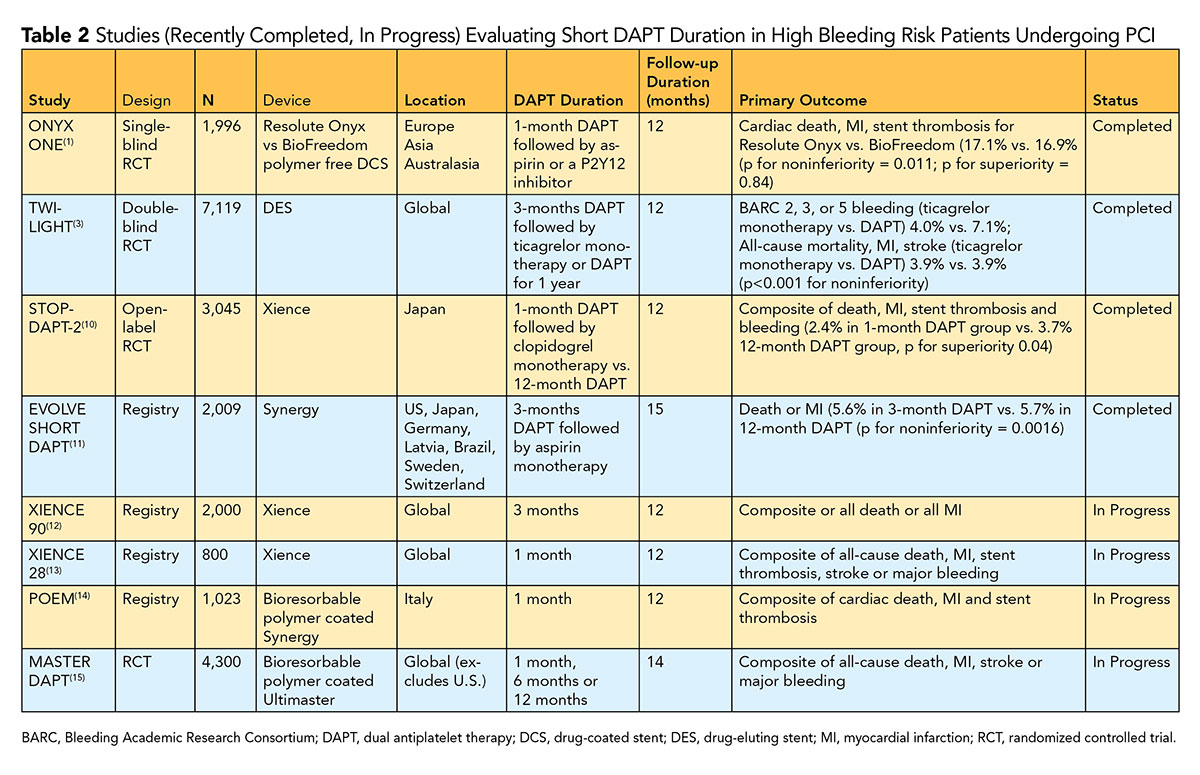
Findings from these studies are likely to change practice as routine use of intracoronary BMS in HBR patients is strongly discouraged and there does not appear to be an advantage to using polymer-free drug-coated stents instead of standard polymer-based drug-eluting stents.
Summary
A large proportion of patients undergoing PCI are considered at high bleeding risk. Striking a judicious balance between risks of ischemia and bleeding in these patients is often challenging.
Although historically BMSs were used in these patients in an effort to minimize DAPT duration, recent studies have demonstrated that a short DAPT duration (one to three months) post PCI with DES is safe and effective in this patient population.
With emerging evidence, BMS is no longer recommended for these patients and the role of polymer-free or bioabsorbable polymer-coated stents in lieu of standard DES is being investigated.
References
- Windecker S, Latib A, Kedhi E, et al. Polymer-based or polymer-free stents in patients at high bleeding risk. N Engl J Med 2020;Feb 12:[Epub aheas of print].
- Mauri L, Kereiakes DJ, Yeh RW, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155-66.
- Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the Academic Research Consortium for High Bleeding Risk. Eur Heart J 2019;40:2632-53.
- Valle JA, Shetterly S, Maddox TM, et al. Postdischarge bleeding after percutaneous coronary intervention and subsequent mortality and myocardial infarction: Insights from the HMO Research Network-Stent Registry. Circ Cardiovasc Interv 2016;9(6).
- Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet 2013;382:614-23.
- Choi SY, Kim MH, Cho YR, et al. Performance of PRECISE-DAPT score for predicting bleeding complication during dual antiplatelet therapy. Circ Cardiovasc Interv 2018;11:e006837.
- Valgimigli M, Patialiakas A, Thury A, et al. Zotarolimus-eluting versus bare-metal stents in uncertain drug-eluting stent candidates. J Am Coll Cardiol 2015;65:805-15.
- Urban P, Meredith IT, Abizaid A, et al. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med 2015;373:2038-47.
- Varenne O, Cook S, Sideris G, et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet 2018;391:41-50.
- Watanabe H, Domei T, Morimoto T, et al. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI: The STOPDAPT-2 randomized clinical trial. JAMA 2019;321:2414-27.
- Kirtane AJ. EVOLVE Short DAPT: A single-arm study of 3-month dapt in patients at high bleeding risk treated with a bioabsorbable polymer-based everolimus-eluting stent. Presentation at TCT 2019. San Francisco.
- XIENCE 90: A Safety evaluation of 3-month DAPT after XIENCE implantation for HBR patients. Available here.
- XIENCE 28 Global Study. Available here.
- Bioresorbable Polymer-Coated EES in Patients at High Bleeding Risk Undergoing PCI Followed by 1-Month DAPT. Available here.
- Management of High Bleeding Risk Patients Post Bioresorbable Polymer Coated Stent Implantation With an Abbreviated Versus Prolonged DAPT Regimen. Available here.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Invasive Cardiovascular Angiography and Intervention, Anticoagulation Management and ACS, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Interventions and ACS
Keywords: ACC Publications, Cardiology Magazine, Drug-Eluting Stents, Platelet Aggregation Inhibitors, Aspirin, Warfarin, Acute Coronary Syndrome, Absorbable Implants, Risk Factors, Incidence, Atrial Fibrillation, Anti-Inflammatory Agents, Non-Steroidal, Patient Discharge, Percutaneous Coronary Intervention, Coronary Vessels
< Back to Listings