Geriatric Conditions in Older Adults with Heart Failure: Part 4. Components of Deprescribing
Click to access: Part 1 | Part 2 | Part 3 | Part 4
Mr. C is an 85-year-old male referred in 2017 for a second opinion with cardiology for episodic "whiteouts." [Original patient case scenario here].
Case Question #4: What are the components of the deprescribing process?
Show Answer
The correct answer is: 4. All of the above.
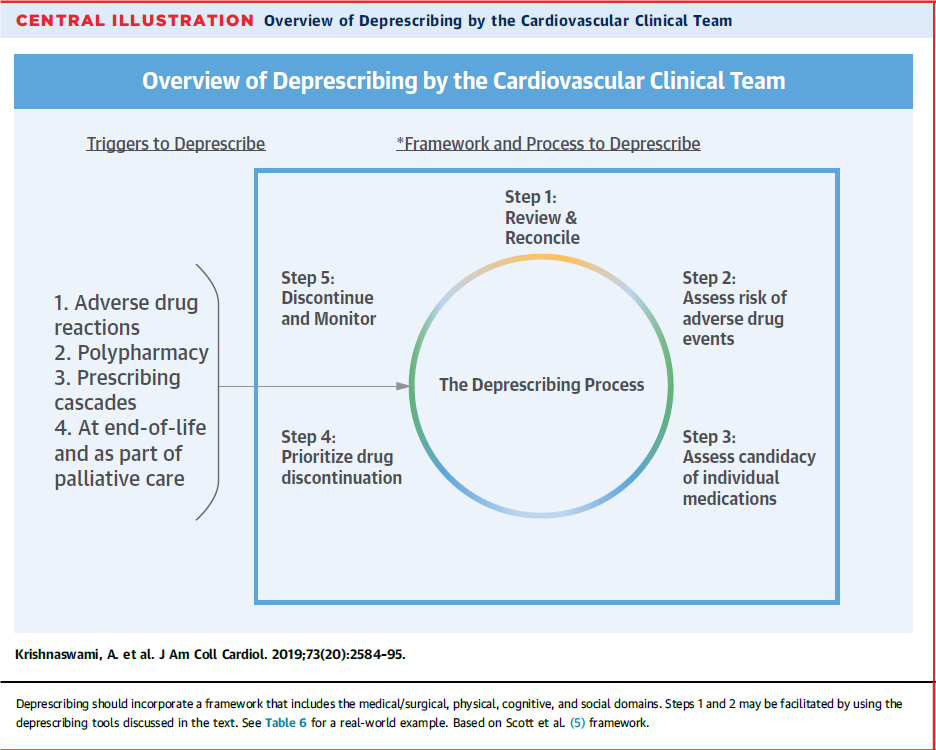
The deprescribing components include the following: triggers, framework, and process. Of note, an adverse drug event can be a current event or an expected future event based on the clinical scenario. The deprescribing components are illustrated below:1
Figure 1
The 5-step deprescribing process for Mr. C specifically is as follows:
Step 1: Medication review and reconciliation.
Specifically, vitamins and supplements (vitamin D3/calcium supplements, vitamin E and fish oil) were felt to have no specific indications for improving survival or decreasing symptoms. Ferrous sulfate was prescribed over 10 years ago due to an upper gastrointestinal bleed.
Step 2: Individual medication risk assessment for current or future adverse effects.
Adverse effects from carvedilol, losartan, furosemide and spironolactone were felt to be contributing to his symptoms. Supplements did not contribute to symptoms but added burden of polypharmacy. Ferrous sulfate was thought to be causing frequent severe constipation.
Step 3: Assessment of candidacy for individual medication discontinuation.
It was felt that the four aforementioned heart failure medications will need to be removed or the dose decreased substantially through close monitoring of symptoms, blood pressure, weight, fluid and solids input through gastrostomy tube.
The blood pressure goal determined was the systolic blood pressure where he had no symptoms of "whiteouts." Ferrous sulfate was considered for removal due to adverse effect as described above and stable hemoglobin level for many years of 12-13g/dl. Aspirin was considered for removal due to no obvious increase in improving survival or decrease of symptoms in non-ischemic cardiomyopathy.
Step 4: Establishing drug discontinuation prioritization.
With an understanding of volume status (knowledge of input and weight), the prioritization was to decrease spironolactone dose. Then decrease, discontinue, and possibly switch carvedilol to another β-blocker with less propensity for hypotension. Lastly, losartan was decreased to 12.5 mg daily. Simultaneous priority was to remove ferrous sulfate and aspirin.
Step 5: Establishing a protocol for discontinuation and monitoring.
After informed consent, the above plan was executed, and patient closely monitored with regular video conferencing visits and occasional clinic visits over a period of 6 months.
At these visits, symptoms, blood pressure, pulse, weight, and medication use were routinely assessed. Final CV medications (doses): bisoprolol (2.5-mg), furosemide (20-mg as needed only, based on weight changes), aldactone (12.5-mg), losartan (12.5 mg).
Follow Up of Mr. C:
At a blood pressure ≥130-135 mmHg patient did not have any further "whiteouts." He was able to spend three consecutive summers at his vacation home. As of September 2020, Mr. C had two hospitalizations in 2018 (one for pleural effusion necessitating a daily and increase in diuretic dose) and the second for epistaxis. He has subsequently not returned to the hospital.
It is noteworthy that in this case, Mr. C experienced severe adverse effects from polypharmacy/medication overload. The medications prescribed were based on current recommendations for management of heart failure. It is important that the cardiovascular team (CVT) focus on patient-centric goals of care (What Matters Most2) when caring for older, multimorbid adults with cardiovascular diseases. Moreover, the CVT should feel comfortable to deprescribe medications based on the ethical principles previously described. Consultation with geriatric cardiologists or geriatricians may aid in this process.
References
- Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol 2019;73:2584-95.
- Tinetti M, Huang A, Molnar F. The Geriatrics 5M's: a new way of communicating what we do. J Am Geriatr Soc 2017;65:2115.
Click to access: Part 1 | Part 2 | Part 3 | Part 4

