Evaluating Variations in Secondary Prevention of Coronary Heart Disease: The INTERASPIRE Study
Quick Takes
- Guideline-endorsed secondary-prevention measures reduce recurrent adverse events in individuals with coronary artery disease.
- The INTERASPIRE (International Action on Secondary Prevention through Intervention to Reduce Events) study results expand on previous research regarding global implementation and adherence to secondary-prevention measures.
- The age-standardized and sex-standardized prevalence of optimal guideline adherence was just 1% in the INTERASPIRE cohort, highlighting geographic and sex disparities and the need for standardization.
Background
Coronary artery disease (CAD) affected >315 million people worldwide in 2022.1 Individuals with CAD have a 20% increased 5-year risk of adverse cardiac events.2,3 Secondary-prevention measures to reduce risk are paramount, but implementation and adherence remain uncertain. Previous studies—including EUROASPIRE I (European Action on Secondary and Primary Prevention by Intervention to Reduce Events I), EUROASPIRE II (European Action on Secondary and Primary Prevention by Intervention to Reduce Events II), PURE (Prospective Urban Rural Epidemiology), STABILITY (Stabilization of Atherosclerotic Plaque by Initiation of Darapladib Therapy), and CLARIFY (Prospective Observational Longitudinal Registry of Patients With Stable Coronary Artery Disease)—investigated compliance with preventive measures targeting CAD risk factors (Table 1).4-7
Table 1: Summary of the Main Findings of Previous Studies of Preventive Measures Targeting CAD Risk Factors
|
Study
|
Time Frame
|
Demographics
(% Female, Age [Years]) |
Main Findings
|
| EUROASPIRE I4 (N = 3,569) |
1995-1996 | 25, 61 | Overall adverse lifestyle habits:
|
| EUROASPIRE II4 (N = 3,379) |
1999-2000 | 25, 61 | Persistent adverse lifestyle trends:
|
| PURE5 (N = 153,996) |
2003-2009 | 58.4, 49.8 ± 9.7 (female) and 50.8 ± 9.8 (male) | Low prevalence of secondary-prevention medication use and disproportionately favoring high-income countries:
|
| STABILITY6 (N = 15,828) |
2008-2013 | 19, 64.4 ± 9.4 | Many patients have modifiable risk factors and failed to meet secondary-prevention goals:
|
| CLARIFY7 (N = 32,703) |
2009-2010a | 22.4, 64.2 ± 10.5 | High-risk groups benefit from more intensive treatment:
|
ACEi = angiotensin-converting enzyme inhibitor; AF = atrial fibrillation; ARB = angiotensin-receptor blocker; BP = blood pressure; CAD = coronary artery disease; CLARIFY = Prospective Observational Longitudinal Registry of Patients With Stable Coronary Artery Disease; CV = cardiovascular; DM = diabetes mellitus; EUROASPIRE = European Action on Secondary and Primary Prevention by Intervention to Reduce Events; MI = myocardial infarction; PAD = peripheral artery disease; PURE = Prospective Urban Rural Epidemiology; STABILITY = Stabilization of Atherosclerotic Plaque by Initiation of Darapladib Therapy; TC = total cholesterol.
The EUROASPIRE I and II study results showed worsening adverse lifestyle practices, with failures in implementation of secondary-prevention guidelines.4 The PURE study results highlighted health disparities in low socioeconomic areas.5 The STABILITY study results showed that most patients with chronic CAD did not meet secondary-prevention goals.6 The CLARIFY registry investigators noted previous trial limitations, citing their outdated nature and changes in CAD characteristics.7 More intensive guidelines, inadequate risk stratification, and lack of standardization between studies requires further attention.3
The INTERASPIRE (International Action on Secondary Prevention through Intervention to Reduce Events) study aimed to address these knowledge gaps by assessing contemporary implementation of secondary-prevention guidelines on the basis of the European Society of Cardiology (ESC) EUROASPIRE research program.3
Methods
Between March 2020 and May 2023, the INTERASPIRE study retrospectively identified 4,548 patients between 18 and 79 years of age from 88 hospitals across 14 countries in all six World Health Organization (WHO) regions—Africa, the Americas, Eastern Mediterranean, Europe, Southeast Asia, and Western Pacific—and assessed implementation of guideline-based risk-factor management and lifestyle modifications.3 Patients were included if they had experienced an ST-segment elevation myocardial infarction/non−ST-segment elevation myocardial infarction (STEMI/NSTEMI), coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), unstable angina (UA), or acute myocardial infarction (AMI) 6-24 months earlier (36 months in Africa).3
Self-reported information on lifestyle practices, risk-factor management, medications, and rehabilitation was obtained. Standardized assessments included smoking status, height, and weight with calculated body mass index, waist circumference, and blood pressure (BP). Fasting blood samples were drawn to measure glucose and lipid levels.3 Results were reported after standardization by age and sex. The primary goals were to assess how well preventive measures were applied in real-world settings and to identify areas of improvement.
Main Findings
At baseline, 66% of patients were <65 years of age (60 ± 10 years) and 21% were female.3 The most common conditions were STEMI (32%), NSTEMI (21%), UA/AMI (29%), elective PCI (21%), and CABG (7%).3 Lifestyle-related risk factors included 13% current smokers, with nearly half (48%) with smoking at the time of a coronary event persisting at the study visit.3 Approximately 68% (72% female, 69% male) of patients presented with overweight, 44% with self-reported diabetes mellitus, 27% with hyperglycemia, and 17% with glomerular filtration rate <60 mL/min/1.73 m2; further, 67% reported leading sedentary lifestyles.3 Target BP (<130/80 mm Hg) was unmet in 61% of patients, and 83% (88% female, 82% male) of patients had elevated low-density lipoprotein cholesterol levels ( ≥1.4 mmol/L [55 mg/dL]).3
Most patients were taking antiplatelet/anticoagulant medications (96%), beta-blockers (79%), renin-angiotensin-aldosterone system medications (68%), or statins (85%).3 Cardiac rehabilitation referrals varied, with 9% of patients attending only half of the recommended sessions and wide variation (0.4-62%) between countries.3 Further analysis showed that 19.6% of patients had a lipoprotein(a) (Lp[a]) level ≥115 nmol/L, with only 2% practicing a healthy lifestyle.8 Of note, higher Lp(a) levels were observed in women, patients with chronic kidney disease, those with arterial disease, and those taking proprotein convertase subtilisin/kexin type 9 inhibitors.8 Overall, most patients did not reach optimal guideline-recommended thresholds.
Implications
The INTERASPIRE study results demonstrated a failure in secondary prevention of CAD worldwide,3 consistent with the EUROASPIRE, CLARIFY, and PURE results. Importantly, the INTERASPIRE study data provide contemporary updates using the most recent guideline targets, showing poorer glucose level and BP control in female patients.3-7 The study data also showed that less than one-half of participants were taking optimal guideline-directed therapy.3 Notably, two-thirds of participants were not meeting guideline-recommended physical activity targets.3 Unlike its predecessors, the INTERASPIRE study provided information on the timely implementation of these risk-factor targets with a median of 1-year implementation after diagnosis.3 This findings raises a critical concern about the effectiveness of prevention-strategy implementation and adherence, particularly with the lack of improvement since the initial pilot studies.
The strengths of this study include high-quality worldwide data, large sample size, and cohort diagnosis consistency with the EUROASPIRE program. The study's limitations include globally nonrepresentative geographic areas and the coronavirus disease 2019 pandemic, which limited face-to-face interviews/examinations and provided recruitment challenges.
In summary, secondary prevention of CAD was significantly below standard guideline recommendations, with large variations between countries and sex (Figure 1). These findings offer insight into the need for urgent standardized and evidence-based prevention measures globally. Future studies should include a larger cohort, incorporating patients from more geographic areas, a wider age range, and a higher representation of female sex.
Figure 1: Results of Secondary-Prevention Guideline Targets for CAD
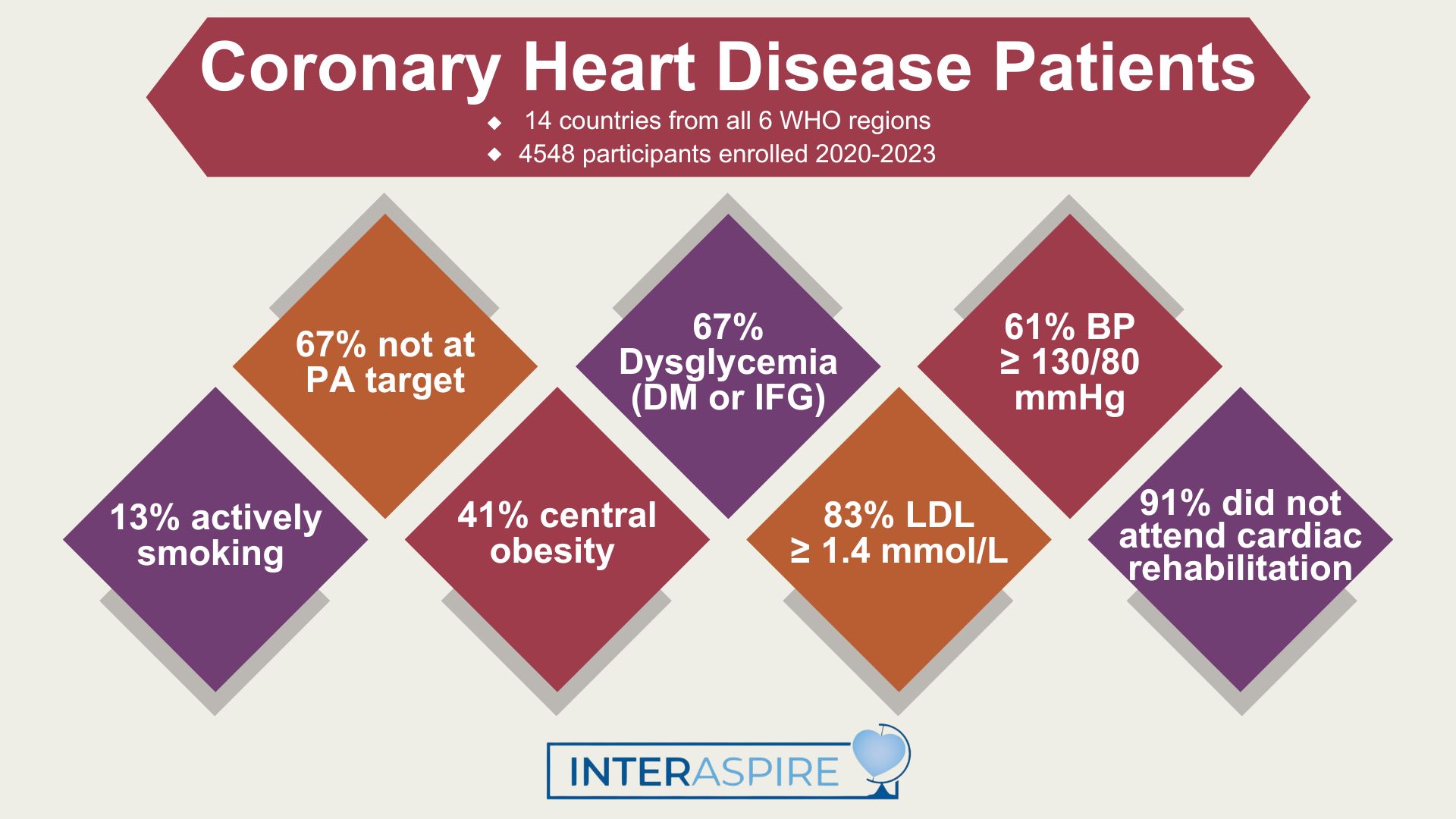
BP = blood pressure; CAD = coronary artery disease; DM = diabetes mellitus; IFG = impaired fasting glycemia; INTERASPIRE = International Action on Secondary Prevention through Intervention to Reduce Events; LDL = low-density lipoprotein; PA = physical activity; WHO = World Health Organization.
References
- Stark B, Johnson C, Roth GA. Global prevalence of coronary artery disease: an update from the global burden of disease study. J Am Coll Cardiol 2024;83:2320.
- Kerr AJ, Broad J, Wells S, Riddell T, Jackson R. Should the first priority in cardiovascular risk management be those with prior cardiovascular disease? Heart 2009;95:125-9.
- McEvoy JW, Jennings C, Kotseva K, et al. Variation in secondary prevention of coronary heart disease: the INTERASPIRE study. Eur Heart J 2024;45:4184-96.
- EUROASPIRE I and II Group, European Action on Secondary Prevention by Intervention to Reduce Events. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. Lancet 2001;357:995-1001.
- Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE study): a prospective epidemiological survey. Lancet 2011;378:1231-43.
- Vedin O, Hagström E, Stewart R, et al. Secondary prevention and risk factor target achievement in a global, high-risk population with established coronary heart disease: baseline results from the STABILITY study. Eur J Prev Cardiol 2013;20:678-85.
- Sorbets E, Fox KM, Elbez Y, et al. Long-term outcomes of chronic coronary syndrome worldwide: insights from the international CLARIFY registry. Eur Heart J 2019;41:347-56.
- Ray KK. INTERASPIRE: A global perspective of Lp(a) levels in patients with coronary heart disease — Implications for risk factor control & future trials from the INTERASPIRE Study (National Institute for Prevention and Cardiovascular Health website). 2024. Available at: https://nipc.ie/interaspire-a-global-perspective-of-lpa-levels/. Accessed 11/23/2024.
Clinical Topics: Cardiovascular Care Team, Prevention, Atherosclerotic Disease (CAD/PAD), Acute Coronary Syndromes, Dyslipidemia, Diabetes and Cardiometabolic Disease
Keywords: Coronary Artery Disease, Secondary Prevention, Life Style, Guideline Adherence, Guideline, Guidelines as Topic
