Advancing DEI In Cardiology Fellowship Recruitment, Improving CV Care and Outcomes
Cardiology training programs in the U.S. lack a standardized approach to considering diversity, equity and inclusion (DEI) when selecting fellows. In an article published Sept. 23 in JACC, Daniel Amponsah, MD, and Celia M. Yong, MD, FACC, discuss the positive impacts of DEI in terms of patient care and outcomes and propose a framework for integrating DEI principles into the selection process for cardiology fellowship.
In addition to justice, they state, there is a large body of evidence showing that diversity within medicine has clinical and economic benefits. For example, concordance between patient-provider sex and race is associated with lower mortality, increased patient satisfaction and improved health care delivery. Furthermore, such concordance can lower emergency department use and total health care expenditures. Notably, research also shows that “a diverse workforce can produce pleiotropic effects for all providers and patients regardless of individual race or sex.”
Currently, the field of cardiology ranks among the worst in medicine for racial and gender diversity. Among cardiology fellows in the U.S., only 24.6% are women and 11.8% are from minoritized backgrounds. Although some leading cardiology fellowship programs in the U.S. have implemented strategies to improve DEI, many programs still lack a standardized approach to prioritizing DEI in the selection process.
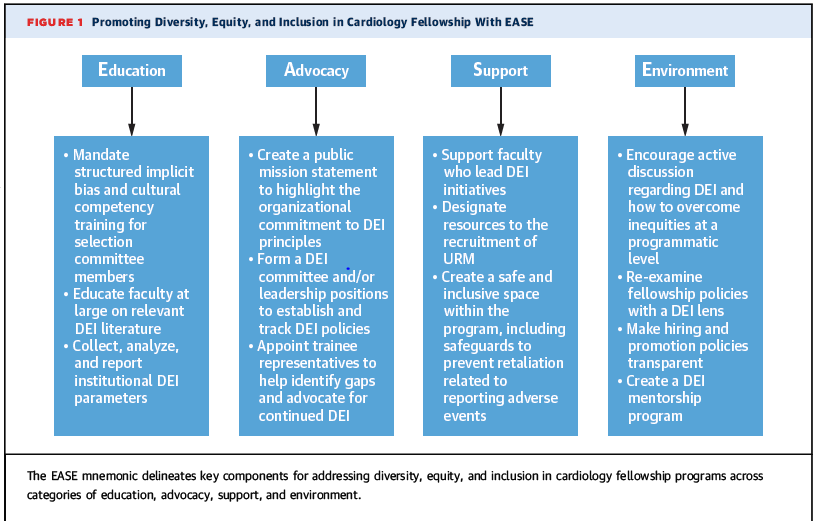
The authors write that “a commitment to building a culture that emphasizes DEI is essential to establishing an equitable and supportive training environment.” Along with a clear mission statement, transparency about concrete initiatives, training on implicit bias and cultural competency for members of all relevant committees, they propose adoption of the Education, Advocacy, Support, Environment (EASE) framework, which delineates key components for addressing DEI in fellowship programs across those categories. They write that programs can be held accountable by “committing to the collection, reporting, and analysis of annual DEI metrics to foster a culture of continuous improvement and inclusivity with the program.”
In an accompanying response, Jennifer H. Mieres, MD, FACC, and Paul L. Douglass, MD, MACC, write that “a multipronged approach and actionable implementation plan are critical to enhance and sustain the tenets of DEI into the cardiology training model.” This includes the call to action from Amponsah and Yong for the “active engagement and advocacy of cardiovascular medical societies to collaborate with training programs to diversify the cardiovascular workforce.”
Mieres and Douglass challenge the authors to add an accountability strategy to monitor the progress of the EASE framework, which could benefit the cardiovascular training community and track the impact of the integration of DEI with cardiovascular health outcomes. “This call underscores the urgency for change to reaffirm our commitment to health equity and social justice,” they write.
Keywords: Cultural Competency, Health Equity, Patient Care, Social Justice
