Latest in ED Risk Stratification of Chest Pain: hs-cTn and Risk Scores
Quick Takes
- Most patients who rule-out for myocardial infarction (MI) with very low levels of high-sensitivity cardiac troponin (hs-cTn) at presentation, or not changing significantly at 1-2 hours, can be discharged from the emergency department (ED) without further cardiac testing (stress testing or imaging).
- Patients with intermediate hs-cTn values can have the HEART (History, ECG, Age, Risk Factors, Troponin) or EDACS (Emergency Department Assessment of Chest Pain Score) score utilized to assist in disposition.
Introduction
Evaluation of patients in the ED for possible MI remains a major concern. In a survey of ED physicians, the acceptable risk for major adverse cardiac events (MACE) (death/MI) soon after discharge was <0.5%.1 Algorithms using very low levels of hs-cTn at presentation, or the lack of change at low levels within 1-2 hours, enables MI to be excluded rapidly. Risk scores have been developed to help in prognostication of patients evaluated in the ED for possible MI; their use is an established part of care in many institutions. However, the prognostic utility of low-level hs-cTn measurements (well below the 99th percentile) has supplanted some of the clinical applicability of these risk scores.2
Risk Scores
Some of the most cited risk scores are the HEART, EDACS, GRACE (Global Registry of Acute Coronary Events), and TIMI (Thrombolysis in Myocardial Infarction) scores. The GRACE and TIMI scores were derived from trials involving patients with definite acute coronary syndrome and have not prognostically performed as well in patients evaluated with chest pain of unclear etiology.3,4 The HEART and EDACS scores, however, were developed to risk stratify patients with chest pain of unclear etiology and are superior to the TIMI and GRACE scores in this regard.5,6 Elements of the EDACS and HEART scores are shown in Table 1.
Table 1: HEART and EDACS Scores
| HEART Components (Low risk ≤3) | EDACS Components (Low risk ≤15) | ||
| History: | Age: | ||
| High suspicion | 2 | 18-45 | 2 |
| Moderate suspicion | 1 | 46-50 | 4 |
| Low suspicion | 0 | 51-55 | 6 |
| Electrocardiogram: | 56-60 | 8 | |
| ST-segment deviation | 2 | 61-65 | 10 |
| Paced, left bundle branch block, right bundle branch block, or left ventricular hypertrophy | 1 | 66-70 | 12 |
| Normal or nonspecific changes | 0 | 71-75 | 14 |
| Age: | 76-80 | 16 | |
| >65 | 2 | 81-85 | 18 |
| 45-65 | 1 | 86+ | 20 |
| <45 | 0 | Male sex | 6 |
| Cardiac risk factors, i.e., hypertension, diabetes mellitus, current tobacco abuse, family history of coronary artery disease (history of prior MI, percutaneous coronary intervention, coronary artery bypass graft, or left main artery >50% or other coronary artery >70% stenosis): | Age 18-15 and either ≥3 cardiac risk factors or known coronary artery disease (previous acute MI, coronary artery bypass graft, or percutaneous coronary intervention) | 4 | |
| ≥3 risk factors or known coronary artery disease | 2 | Diaphoresis | 3 |
| 1-2 risk factors | 1 | Pain radiating to arm or shoulder | 5 |
| 0 risk factors | 0 | Pain worsened with inspiration | -4 |
| Pain reproduced by palpation | -6 | ||
| Each component is summed to give a final score | |||
There have been no prospective trials comparing EDACS to HEART, so neither score is clearly superior to the other. The prognostic ability of low-level hs-cTn measurements lessens the need for the use of risk scores. The use of the newer algorithms allows MI to be excluded in 3 ways:
- Very low levels at presentation (near or at the level of detection)
- Low levels at presentation but not changing significantly at 1-2 hours
- Serial values ≤99th percentile over 3 hours
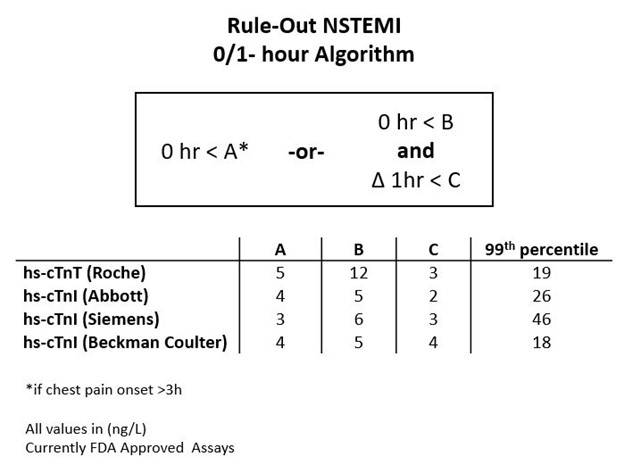
Because there is no standardization among various hs-cTn assays, the actual numbers used in the protocols are different (Figure 1).
Figure 1: Rule-Out Non-ST-Segment Elevation MI
Rule-Out MI
Rule-Out at Presentation
In a meta-analysis of 22,457 patients from 19 studies, 49.1% of patients had a hs-cTnI <5 ng/L, and the 30-day MACE rate was 0.5%.7 A recent multicenter randomized study of 31,492 patients compared a rapid rule-out strategy at presentation with hs-cTnI <5 ng/L to serial hs-cTnI over 6-12 hours after symptom onset. There was no significant difference between 30-day cardiac death/MI between the strategies: 0.3% in the rapid strategy and 0.4% in the standard strategy.8 Thus, patients with very low levels at presentation are highly unlikely to suffer an acute MI and are at very low risk for 30-day MACE. Risk scores are not needed in patients with very low hs-cTn levels at presentation.
Rule-Out by 0/1-Hour Algorithm
Most studies evaluating the 0/1-hour algorithm have been retrospective. One retrospective study of the 0/1-hour algorithm with 1,282 patients using the hs-cTnT assay applied the HEART score.9 The HEART score was able to distinguish between very low-risk and higher-risk patients. Those with a HEART score ≤3 had a 30-day MACE rate of only 0.2%; those with a HEART score ≥4 had a MACE rate of 2.3%. A prospective study involving 2 centers used the 0/1-hour algorithm for actual patient care.10 This study involved 2,296 patients, and 62% of the patients met the criteria for rule-out. In the rule-out group, 71% of patients were discharged for outpatient management. At 30 days in the rule-out group, the MACE rate was 0.2%. There was no formal risk score applied in this study. A prospective randomized trial of 3,378 patients comparing a 0/1-hour to 0/3-hour algorithm demonstrated no difference in 30-day MACE between the 2 groups (0.6% in 0/3-hour group and 0.4% in the 0/1-hour group).11 Calculation of the HEART and EDACS scores was done and available to the clinicians, but use of the scores in medical decision-making was not mandated. What remains unclear is whether a formal risk score is required or whether clinical judgement is enough, upon reviewing the history and electrocardiogram, to decide on the disposition of patients that rule-out by the 0/1-hour algorithm. Similar algorithms have been developed with various assays for 0/2-hour algorithms.12,13 A European Society of Cardiology task force recommends that patients who rule-out within 1 hour be discharged for outpatient evaluation.14 We believe that the use of a formal risk score in those who rule-out by the 0/1-hour algorithm is optional.
Rule-Out by 0/3-Hour Algorithm
Patients with intermediate hs-cTn values who do not rule out at presentation or by the 0/1-hour algorithm require at least a 3-hour value ≤99th percentile to exclude MI. This population is likely to benefit from the application of a risk score. In a prospective implementation study of the HEART score involving 4,761 patients, 30.7% were deemed low risk and considered for discharge if their HEART score was ≤3 and serial hs-cTn was <99th percentile over 3 hours.15 The 30-day MACE rate was 0.4%. In a meta-analysis of studies of the EDACS score that included 11,578 patients, 55% identified as low risk with a 30-day MACE rate of 0.5 %.16 In patients with intermediate hs-cTn elevation (who do not rule-out at presentation or with the 0/1-hour algorithm but have values at 3 hours ≤99th percentile), a risk score can be applied to assist in risk stratification and patient disposition.
The Very Near Future: Practical Implications
The American College of Cardiology and American Heart Association guidelines from 2014 recommend that many patients evaluated in the ED for possible MI be held for a period of observation followed by cardiac testing.17 These recommendations are clearly outdated. The use of low-level hs-cTn algorithms over 1-2 hours will allow many patients to be immediately discharged from the ED for outpatient evaluation. The prognostic utility of formal risk scores will be lessened. New guidelines will be forthcoming within the year that reflect these advances.
References
- Than M, Herbert M, Flaws D, et al. What is an acceptable risk of major adverse cardiac event in chest pain patients soon after discharge from the Emergency Department?: a clinical survey. Int J Cardiol 2013;166:752-4.
- Neumann JT, Twerenbold R, Ojeda F, et al. Application of High-Sensitivity Troponin in Suspected Myocardial Infarction. N Engl J Med 2019;380:2529-40.
- Gibbs J, deFilippi C, Peacock F, et al. The utility of risk scores when evaluating for acute myocardial infarction using high-sensitivity cardiac troponin I. Am Heart J 2020;227:1-8.
- Ruangsomboon O, Thirawattanasoot N, Chakorn T, et al. The utility of the 1-hour high-sensitivity cardiac troponin T algorithm compared with and combined with five early rule-out scores in high-acuity chest pain emergency patients. Int J Cardiol 2021;322:23-8.
- Sakamoto JT, Liu N, Koh ZX, et al. Comparing HEART, TIMI, and GRACE scores for prediction of 30-day major adverse cardiac events in high acuity chest pain patients in the emergency department. Int J Cardiol 2016;221:759-64.
- Poldervaart JM, Langedijk M, Backus BE, et al. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol 2017;227:656-61.
- Chapman AR, Lee KK, McAllister DA, et al. Association of High-Sensitivity Cardiac Troponin I Concentration With Cardiac Outcomes in Patients With Suspected Acute Coronary Syndrome. JAMA 2017;318:1913-24.
- Anand A, Lee KK, Chapman AR, et al. High-Sensitivity Cardiac Troponin on Presentation to Rule Out Myocardial Infarction: A Stepped-Wedge Cluster Randomized Controlled Trial. Circulation 2021;Mar 23:[Epub ahead of print].
- McCord J, Cabrera R, Lindahl B, et al. Prognostic Utility of a Modified HEART Score in Chest Pain Patients in the Emergency Department. Circ Cardiovasc Qual Outcomes 2017;10:e003101.
- Twerenbold R, Costabel JP, Nestelberger T, et al. Outcome of Applying the ESC 0/1-hour Algorithm in Patients With Suspected Myocardial Infarction. J Am Coll Cardiol 2019;74:483-94.
- Chew DP, Lambrakis K, Blyth A, et al. A Randomized Trial of a 1-Hour Troponin T Protocol in Suspected Acute Coronary Syndromes: The Rapid Assessment of Possible Acute Coronary Syndrome in the Emergency Department With High-Sensitivity Troponin T Study (RAPID-TnT). Circulation 2019;140:1543-56.
- Nowak RM, Christenson RH, Jacobsen G, et al. Performance of Novel High-Sensitivity Cardiac Troponin I Assays for 0/1-Hour and 0/2- to 3-Hour Evaluations for Acute Myocardial Infarction: Results From the HIGH-US Study. Ann Emerg Med 2020;76:1-13.
- Boeddinghaus J, Reichlin T, Cullen L, et al. Two-Hour Algorithm for Triage toward Rule-Out and Rule-In of Acute Myocardial Infarction by Use of High-Sensitivity Cardiac Troponin I. Clin Chem 2016;62:494-504.
- Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care 2020;9:76-89.
- Mahler SA, Lenoir KM, Wells BJ, et al. Safely Identifying Emergency Department Patients With Acute Chest Pain for Early Discharge. Circulation 2018;138:2456-68.
- Boyle RSJ, Body R. The Diagnostic Accuracy of the Emergency Department Assessment of Chest Pain (EDACS) Score: A Systematic Review and Meta-analysis. Ann Emerg Med 2021;77:433-41.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139-e228.
Clinical Topics: Acute Coronary Syndromes
Keywords: Chest Pain, Myocardial Infarction, Troponin, Prospective Studies, Retrospective Studies, Patient Discharge, Acute Coronary Syndrome, American Heart Association, Troponin I, Electrocardiography, Emergency Service, Hospital, Registries, Risk Assessment, Risk Factors, Thrombolytic Therapy
< Back to Listings