Ten Points to Remember: Myocardial Ischemia in Anomalous Aortic Origin of a Left Coronary Artery with an Intraseptal Course
Anomalous aortic origin of the left coronary artery (AAOLCA) with intraseptal (intraconal or transseptal) course is generally considered a benign entity. However, case reports of severe cardiac symptoms such as myocardial ischemia, arrhythmia, and even sudden cardiac death have been sporadically reported.
The following are ten highlighted features from recent publications regarding children with AAOLCA and an intraseptal course.
- Eighteen children with a median age of 12.4 years were followed over approximately 2 years. More than half were asymptomatic at presentation, with equal numbers complaining of non-exertional and exertional symptoms. There were no aborted sudden cardiac deaths nor documented arrhythmias.1
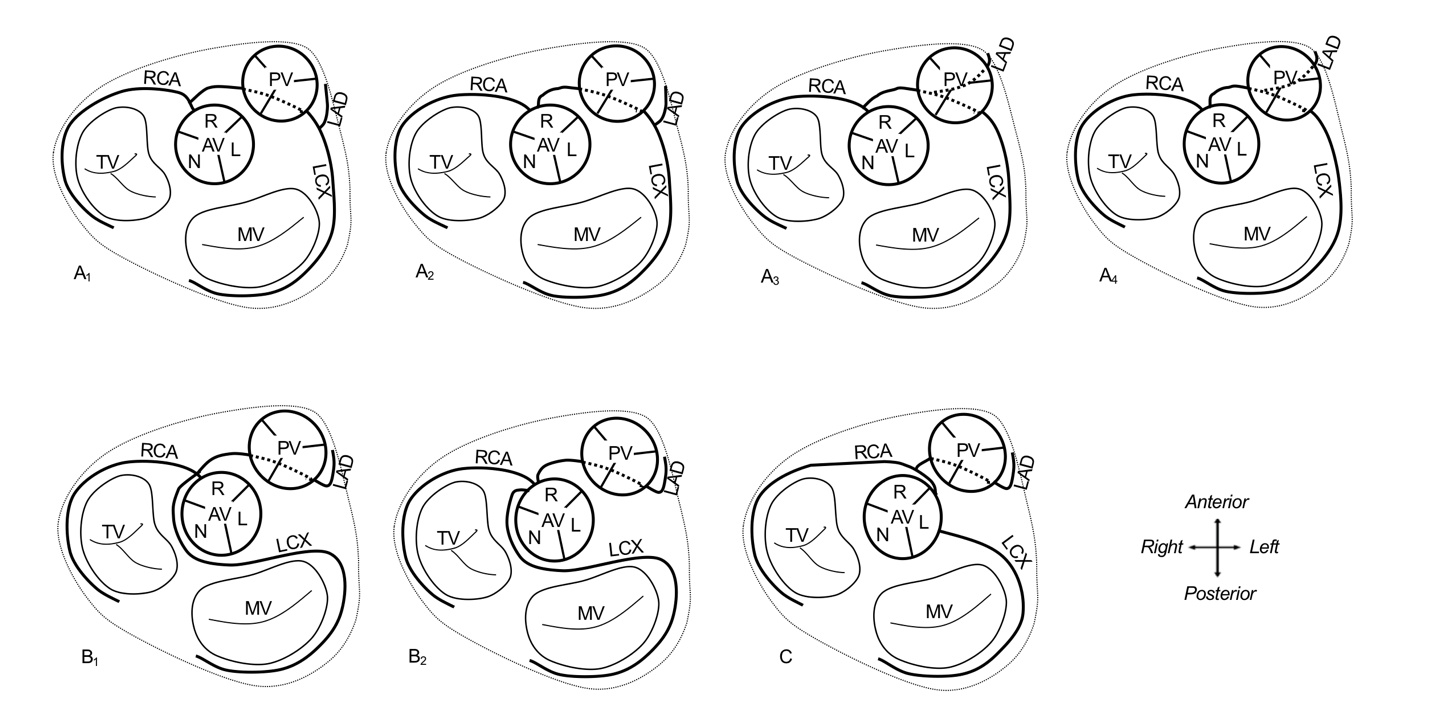
- Computed tomography (CT) angiography was utilized to define coronary origin and course (Figure 1).1 Three major categories were identified (Types A, B, and C). In type A, the left main coronary artery (LMCA) arises from the right sinus, courses intraseptally, and bifurcates after it returns to the epicardium (A1 [single origin] and A2 [separate origins]) or bifurcates within the ventricular septum (A3 [single origin] and A4 [separate origins]). In type B, only the left anterior descending (LAD) artery arises from the right aortic sinus and courses intraseptally, and the left circumflex artery (LCX) arises from the right aortic sinus with a posterior retroaortic course (B1 [single origin] and B2 [separate origins]). In Type C, the LAD arises from the right coronary artery (RCA) with normal origin of the LCX from the left aortic sinus with anomalous aortic origin of the RCA from the left aortic sinus.
Figure 1
- A treadmill exercise stress test (EST) using the Bruce protocol was performed in 13 children older than 8 years of age. Results were normal in six patients, non-specific ST changes were noted in six others, and ST changes concerning for ischemia were noted in one child.1
- Non-invasive perfusion imaging (Stress MRI) was performed in 14 children. Inducible perfusion defects at peak stress were detected in about half of them, four of whom had exertional symptoms.1
- Those with perfusion defects or exertional symptoms concerning for ischemia underwent transcatheter coronary angiography as well as instantaneous wave-free ratio (iFR), and fractional flow reserve (FFR) measurements using dobutamine. A diastolic FFR ≤0.8 during dobutamine and/or baseline instantaneous wave-free ratio ≤0.89 were considered markers for significant coronary flow impairment2 and occurred in slightly over half of the patients.1
- Exertional syncope is a harbinger for a malignant sub-type. Of the two patients who presented with exertional syncope at 5 and 7 years, both had subtype A3 anatomy with long combined intraseptal and intramyocardial length of the LMCA, LAD, and LCX. Both had inducible hypoperfusion defects, reduced iFR (≤0.89), and reduced diastolic FFR at peak dobutamine stress (≤0.8).1
- All patients were discussed at multidisciplinary meetings. Patients <8 years old and with no concern for myocardial ischemia were allowed full exercise participation with periodic follow-up. Shared decision making with the family was employed in the management of patients with concern for myocardial ischemia. Recommendations include exercise restriction, beta-blockade, and surgery.1
- Beta-blockade was considered in patients with reduced iFR (≤0.89) and/or reduced diastolic FFR (≤0.8) at peak dobutamine stress. One of the two patients with subtype A3 was started on atenolol at age 7 with resolution of exertional syncope. Six years later, a repeat dobutamine stress cardiac magnetic resonance imaging (MRI) showed no inducible perfusion defect, iFR of 0.97 (normal >0.89) and diastolic FFR of 0.91 (normal >0.8) during peak dobutamine stress.3
- Surgical intervention was individualized to the patient's anatomy and recommended in those with severe symptoms and/or evidence of myocardial infarction with ongoing ischemia.1,4 One patient with subtype A3 had severe narrowing of the intraseptal LMCA, underwent coronary artery bypass grafting at the age of 5, and was doing well on beta-blockade and antiplatelet therapy with no recurrent syncope.1 A 16-year-old male who presented with exertional chest pain and near syncope was diagnosed with sub-type A1. He had subendocardial delayed enhancement suggestive of prior myocardial infarction and ongoing inducible ischemia on dobutamine stress cardiac MRI, reduced iFR at baseline (0.85), and reduced diastolic FFR with dobutamine (0.69). He underwent a successful supra-arterial myotomy of the intraseptal segment via a right ventriculotomy with direct reimplantation of the LMCA. Following postoperative resolution of inducible myocardial hypoperfusion, the patient was allowed to return to competitive wrestling activities with no further symptoms.4
- Intraseptal anomalous aortic origin of a coronary artery (AAOCA) may have a benign natural history, but generalizations must be avoided. The management of symptomatic patients and those with inducible myocardial ischemia remains challenging due to the complexity of surgical interventions and lack of long-term follow-up data. Collaboration among centers following similar assessment protocols and prospective longitudinal follow-up is essential to manage this rare entity.
References
- Doan TT, Zea-Vera R, Agrawal H, et al. Myocardial ischemia in children with anomalous aortic origin of a coronary artery with intraseptal course. Circ Cardiovasc Interv 2020;13:e008375.
- Doan TT, Wilkinson JC, Agrawal H, et al. Instantaneous wave-free ratio (iFR) correlates with fractional flow reserve (FFR) assessment of coronary artery stenoses and myocardial bridges in children. J Invasive Cardiol 2020;32:176-79.
- Doan TT, Qureshi AM, Sachdeva S, Noel CV, Reaves-O'Neal D, Molossi S. Beta-blockade in intraseptal anomalous coronary artery with reversible myocardial ischemia. World J Pediatr Congenit Heart Surg 2021;12:145-48.
- Doan TT, Molossi S, Qureshi AM, McKenzie ED. Intraseptal anomalous coronary artery with myocardial infarction: novel surgical approach. Ann Thorac Surg 2020;110:e271-74.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Aortic Surgery, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Interventions, CHD and Pediatrics and Quality Improvement, Interventions and Imaging, Interventions and Structural Heart Disease, Angiography, Magnetic Resonance Imaging, Nuclear Imaging
Keywords: Fractional Flow Reserve, Myocardial, Dobutamine, Atenolol, Platelet Aggregation Inhibitors, Coronary Angiography, Sinus of Valsalva, Exercise Test, Ventricular Septum, Follow-Up Studies, Prospective Studies, Decision Making, Myocardial Infarction, Myocardial Infarction, Myocardial Ischemia, Coronary Artery Bypass, Magnetic Resonance Imaging, Death, Sudden, Cardiac, Syncope, Chest Pain, Arrhythmias, Cardiac, Pericardium, Perfusion Imaging, Perfusion, Replantation, Heart Defects, Congenital, Pediatrics
< Back to Listings