Informatics: An Emerging Sub-Specialty in Cardiology
Rallied by the proliferation of rapidly evolving digital technologies, healthcare has joined the movement of digital transformation, involving changes in culture and competencies surrounding digital information technology (IT). Digital transformation is at once promising and problematic for cardiologists in many ways.
The Promises
Digital solutions have potential to make physician efforts more efficient. In patient care, the electronic health record (EHR) makes patient information accessible and easier to store and manage, and can support clinical decision-making through order sets, alerts and reminders, display of clinical guidelines, and data analysis. Patient communication, education, and engagement are enhanced by electronic patient portals that serve an increasingly technology-savvy patient population. Educational smartphone applications with visual aids demonstrating anatomy or procedures are readily at-hand; other apps help patients manage medications, communicate with physicians, or even transmit heart rhythm tracings to their cardiologist. In the critical care setting, real-time acquisition and analysis of patient data can be used to predict acute patient deterioration.1 Telemedicine improves access to healthcare, vital for patients with complex cardiac problems. Quality improvement efforts benefit from an improved ability to maintain and analyze data in EHRs and non-clinical databases, as do research efforts through registries and data networks. EHR analytics can be used to measure organizational performance indicators, optimize billing practices, and provide scheduling solutions.
The Problems
New strategies, however, introduce new challenges. This is particularly problematic in healthcare, where digitalization, when driven by technology experts rather than clinicians, can result in de-emphasis of clinical needs and strategies. The consequent challenges can be so limiting that practitioners may perceive digital solutions as obstacles to patient care.
Lack of Interoperability/Interfaces
Intrinsic to the field of pediatric and congenital cardiology is the need for multiple diagnostic modalities. It is rare that a practice or organization finds a single software solution. Should multiple software solutions be used for these various clinical needs, it is uncommon for these to have the capacity to interface with one another. Without the capacity to transfer data from one program to another, clinicians must perform documentation multiple times in multiple programs, wasting effort and introducing error.
Obstacles to Data-Sharing
Software solutions for data management may benefit organizations individually as they choose what best suits their needs. However, incompatibility between solutions and heterogeneity in data definitions complicates digital data-sharing between organizations for patient care, registries, and research.
The EHR
Advances in the EHR have produced sophisticated programs that can be complex and non-intuitive; physicians require training to accomplish even the most fundamental patient care tasks. Training is time-consuming and costly, and unrelenting software updates render new skills obsolete in a matter of months. The shift from the direct simplicity of thoughts penned on paper to clicking boxes or memorizing non-clinical algorithms and coded phrases is a source of frustration. Compounding frustration is the fact that the responsibility of data entry itself is assigned to physicians, adding to an already-maximized workload, while prompting organizations to eliminate other data-entry resources (e.g. transcription support); physicians who rely on such resources find themselves at a major loss. Modifying physician habits to satisfy software requirements directs physician focus away from patient care. These factors play a dominant role in physician burnout.2
Informatics Solutions
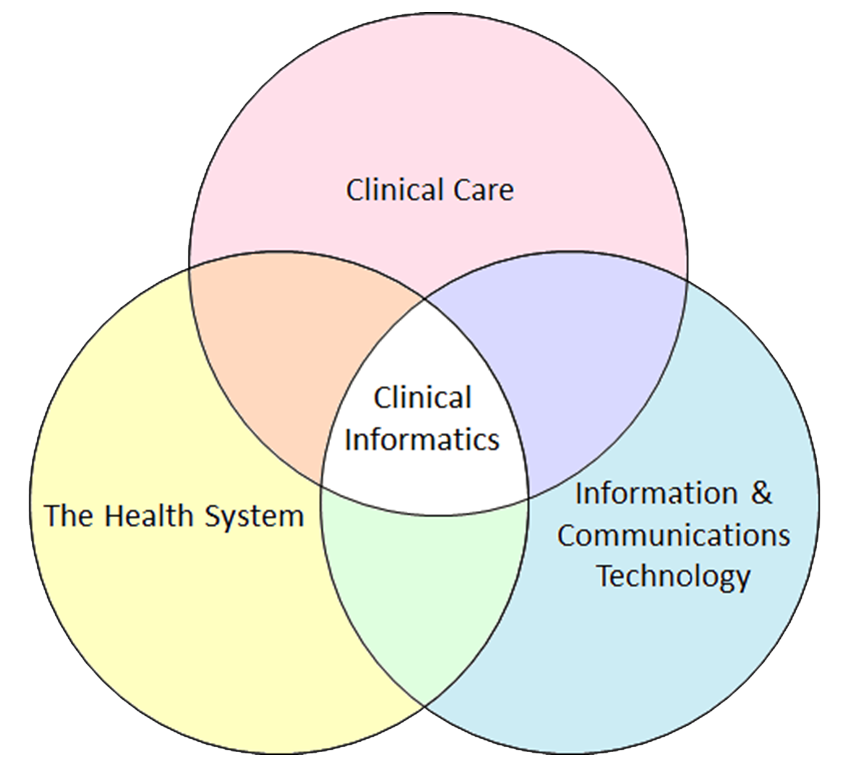
Solutions to address the challenges brought by digitalization lie in informatics. As defined by the American Medical Informatics Association (AMIA), biomedical informatics is "the interdisciplinary field that studies and pursues the effective uses of biomedical data, information, and knowledge for scientific inquiry, problem solving, and decision making, driven by efforts to improve human health."3 Health informatics refers specifically to informatics efforts within healthcare systems. In clinical informatics, the domains of the health system, clinical care, and technology are brought together. [Figure 1]
Figure 1
Results of informatics efforts in cardiology include:
- Standards for reporting templates for cardiac catheterization, heavily involving the EHR5
- The American Heart Association scientific statement on telemedicine, a comprehensive document of the various aspects of telemedicine in cardiology6
- Standardization of data: the creation of key data elements and definitions of a base cardiovascular vocabulary for EHR7 and for cardiovascular endpoints in clinical trials8
The Pandemic
A timely example of the vital role informatics plays is that of the current SARS-CoV-2 pandemic, which has served as a transformative impetus to rapidly implement new technological solutions. It has spurred many practices to build out their telehealth options, involving the redesign of patient scheduling and intake processes in addition to that of visits themselves. As the practice of pediatric cardiology is highly dependent on in-person clinical testing, modifying practice to accommodate telehealth solutions is challenging. Meanwhile, patients and physicians alike must learn new skills to use telehealth platforms with little education or support in the new technologies. ACC.org provides informatics support in the form of guidance for best practices in telehealth, and information on policy and coding/reimbursement.9
Role of the Clinical Informaticist (CI): To Advocate, Educate and Empower
With digital transformation, the need for informatics experts whose role is to identify, create, and implement strategies to serve the data needs of our field has evolved. Ideally suited for this role is the clinician who best understands those needs with respect to our patient population, clinical practices, and research efforts.
The CI advocates for patients and colleagues in unique ways. By helping design and implement digital solutions, the CI helps to ensure that clinical strategies drive the technology, not vice versa, redirecting the focus of physician work back to patient care and away from satisfying software algorithms. Informaticists also coordinate the education and support of their teams in efficient use of technology, including EHRs, empowering teams to utilize data technology to maximize its usefulness.
Recognizing that the CI's role demands a specific knowledge base and skills, the AMIA has published core competencies that the informaticist should posess.3 Historically, physicians have learned informatics through practical experience, but as the field grows, education and board certification in informatics have been formalized.
Currently, two pathways exist to achieve board certification in clinical informatics. The Accreditation Council for Graduate Medical Education (ACGME) has accredited over thirty fellowship programs in Clinical Informatics. In addition, a practice pathway, available until 2022, allows for those physicians with a practical background in informatics to achieve certification without formal fellowship training. Both pathways require passing the clinical informatics subspecialty board examination.
Conclusion
Experts in informatics are needed to lead healthcare practices and organizations through digital transformation, empowering cardiologists to use technology efficiently and to its greatest potential in order to optimize the care of patients with heart disease. Informatics has thus emerged as a vital "subspecialty" within the field.
References
- Rusin CG, Acosta SI, Shekerdemian LS, et al. Prediction of imminent, severe deterioration of children with parallel circulations using real-time processing of physiologic data. J Thorac Cardiovasc Surg 2016;152:171-7.
- Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of heath information technology. J Am Med Inform Assoc 2019;26:106-14.
- Kulikowski CA, Shortliffe EH, Currie LM, et al. AMIA Board white paper: definition of biomedical informatics and specific of core competencies for graduate education in the discipline. J Am Med Inform Assoc 2012;19:931-38.
- Gardner RM, Overhage JM, Steen EB, et al. Core content for the subspecialty of clinical informatics. J Am Med Inform Assoc 2009;16:153-57.
- Sanborn TA, Tcheng JE, Anderson HV, et al. ACC/AHA/SCAI 2014 health policy statement on structured reporting for the cardiac catheterization laboratory: a report of the American College of Cardiology Clinical Quality Committee. J Am Coll Cardiol 2014;63:2591-623.
- Satou GM, Rheuban K, Alverson D, et al. Telemedicine in pediatric cardiology: a scientific statement from the American Heart Association. Circulation 2017;135:e648-e678.
- Weintraub WS, Karlsberg RP, Tcheng JE, et al. ACCF/AHA 2011 key data elements and definitions of a base cardiovascular vocabulary for electronic health records: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards. J Am Coll Cardiol 2011;58:202-22.
- Hicks KA, Tcheng JE, Bozkurt B, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (writing committee to develop cardiovascular endpoints data standards). J Am Coll Cardiol 2015;66:403-69.
- What You Need to Know: Telehealth Services (ACC.org). Available at: https://www.acc.org/latest-in-cardiology/features/accs-coronavirus-disease-2019-covid-19-hub/what-you-need-to-know-about-telehealth-coding-best-practices-and-more-covid-19-coronavirus-disease-2019. Accessed 08/30/2020.
Clinical Topics: Congenital Heart Disease and Pediatric Cardiology, COVID-19 Hub, Congenital Heart Disease, CHD and Pediatrics and Quality Improvement
Keywords: Heart Defects, Congenital, Medical Informatics, American Heart Association, Electronic Health Records, Quality Improvement, Workload, Pandemics, COVID-19, Information Dissemination, Patient Advocacy, Education, Medical, Graduate, Delivery of Health Care, Telemedicine, Patient Care, Accreditation, Knowledge Bases, Audiovisual Aids, Documentation, Reference Standards, Critical Care, Problem Solving, Algorithms, Registries, Cardiac Catheterization
< Back to Listings