Heart Failure Biomarkers in COVID-19
Quick Takes
- Numerous biomarkers may be abnormal in patients with COVID-19, including inflammatory, hematologic, thrombotic and cardiac markers.
- Abnormalities of NT-proBNP and hs-cTn do not necessarily reflect heart failure or acute myocardial infarction.
- Marked elevation or rise in either marker may support clinical judgment regarding involvement of the cardiovascular system and thus support decision making regarding triage and subsequent management, including imaging and physical exam.
Introduction
"Muddy Water, Let Stand, Becomes Clear"
– Lao Tzu, 6th century
With the pandemic spread of the SARS-CoV-2 virus and novel coronavirus disease 2019 (COVID-19), it has been widely observed that traditional biomarkers of heart failure such as cardiac troponins and B-type natriuretic peptides (BNP) are elevated in patients with COVID-19.1-3 Studies suggest infection with SARS-CoV-2 also results in a strong, damaging inflammatory response accompanied by innate immune cell infiltration and hyperinflammation, especially in patients whose host-immune system may not successfully eliminate the virus at disease onset.4,5 This massive immune activation has muddied the water, or rather the serum, and our understanding of elevated markers of myocardial injury remains challenged. In this ACC Expert Analysis, we review the interpretation of biomarkers of heart failure in the context of COVID-19, and perhaps offer a modern interpretation of the Taoist philosophy:
"Cardiac Biomarkers, Let Stand, Become Clear"
This modern interpretation is not, however, without a nuanced understanding of the underlying pathophysiologic pathways these markers represent.
Heart Failure Biomarkers and the Pathophysiologic Pathways They Represent
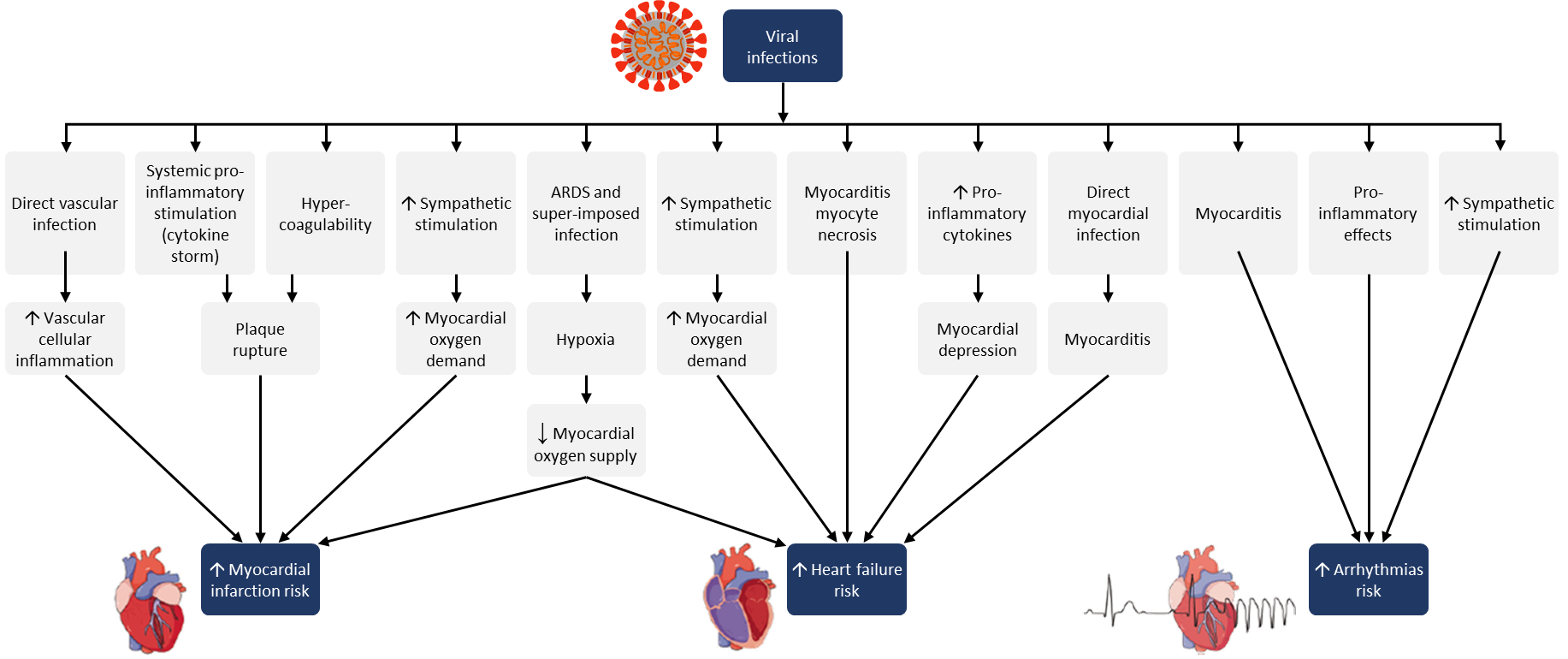
The implications of COVID-19 on the cardiovascular system are numerous. While a host of unique case reports ranging from stress cardiomyopathy to cardiac tamponade have been published,6-8 many postulate that the broader cardiovascular burden of COVID-19 is multifactorial in the setting of severe systemic stress, cytokine storm, acute lung injury and acute respiratory distress syndrome (ARDS).9,10 As such, this critical viral illness is accompanied by multiple stressors including hypoxia, hypotension, increased sympathetic stimulation, a prothrombotic state and systemic pro-inflammatory cytokine storm with sequelae such as increased myocardial oxygen demand, microvascular ischemia, plaque rupture and tachyarrhythmia (Figure 1).
Figure 1: Potential mechanisms for acute effects of viral infections on cardiovascular system
For simplicity purposes, we will consider these pathophysiological changes according to the following rubric of heart failure biomarkers as previously outlined:11 (1) myocardial insult, (2) neurohormonal activation, (3) biomarkers of comorbidity and (4) myocardial remodeling.
Myocardial Insult
Myocardial stress or injury are perhaps the most common conditions under which biomarkers of heart failure have been studied. The vast majority of this data centers around BNP and N-terminal pro-B-type natriuretic peptide (NT-proBNP) as markers of myocardial stretch injury and cardiac troponin as a marker of direct myocyte damage and necrosis. Both BNP/NT-proBNP and cardiac troponin have Class IA indications for heart failure prognosis during hospital admissions, while the use of BNP or NT-proBNP is also recommended for use in diagnosis, prevention, and safe discharge planning for patients hospitalized with heart failure.12 It is of no surprise then that these two biomarkers were some of the earliest described during the coronavirus pandemic.
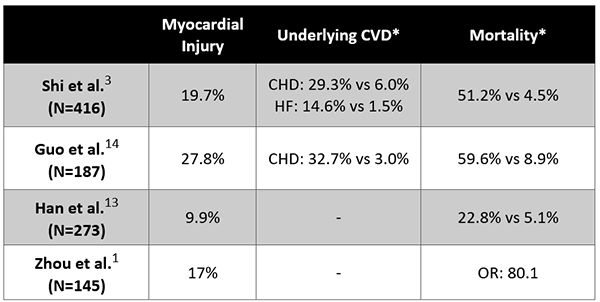
Multiple studies suggest that elevated cardiac biomarker concentrations correlate with disease severity and prognosis in patients with COVID-19, with myocardial injury reported in approximately 10-28% of cases of coronavirus as summarized in Table 1. In one of the early studies out of Wuhan, Zhou et al. described changes in high-sensitivity cardiac troponin I (hs-cTnI) in a comparison of survivors and non-survivors.1 Notably, hs-cTnI increased rapidly from day 16 after disease onset in non-survivors and the odds of in-hospital death were significantly higher in patients with hs-cTnI concentrations >99th percentile (OR 80.1 [95% CI: 10.3–620.4, p<0.0001]). Han, et al. reported similar findings in their study of 273 patients, of which 75 patients were deemed to have severe or critical illness and were found to have significantly elevated levels of both hs-cTnI and NT-proBNP.13 Two additional studies out of China by Shi et al.3 and Guo et al.14 also found that elevations in cTn and NT-proBNP were predictive of disease progression and severity, and additionally identified that patients with pre-existing cardiovascular disease were more likely to develop myocardial injury.
Table 1: Elevated biomarkers of myocardial insult listed by percentage in COVID-19
CVD = cardiovascular disease; CHD = coronary heart disease; HF = heart failure; ARDS = Acute Respiratory Distress Syndrome
Have these studies uncovered a clear and unique cardiovascular correlate with COVID-19? Or, perhaps, have these studies confirmed what is already known to be true about biomarkers of heart failure in critical illness? Studies of cardiac biomarkers in ARDS from various causes (including influenza-like illness) from over a decade ago showed that cTnT concentrations were commonly elevated and strongly predictive of mortality.15 Similarly, in patients with ARDS, NT-proBNP levels were elevated and paralleled severity of clinical syndrome and likelihood for mortality.16 In fact more recently, and prior to the COVID-19 pandemic, this postulate was revisited in over 1,000 patients with ARDS using modern hs-cTn assays in a prospective fashion and again identified myocardial injury in over 90% of patients and a correlation with the degree of critical illness.17
Neurohormonal Activation
It has been well understood for many years that activation of the sympathetic nervous system in heart failure results in upregulation of the renin-angiotensin-aldosterone system (RAAS) and an increase in circulating concentrations of the potent adrenergic neurotransmitters such as epinephrine and norepinephrine.18 With respect to SARS-CoV-2, the RAAS axis poses an interesting physiological correlate as the angiotensin-converting enzyme 2 (ACE2) receptor is the biological target by which SARS-CoV-2 enters lung epithelial cells.19 In fact, ACE2 is expressed broadly in the heart, lungs, and kidneys, and many have postulated a theoretical increase in ACE2 expression among patients using guideline-directed angiotensin-converting enzyme inhibitors or angiotensin receptor blockade.19,20 While this has raised concerns regarding their safety in patients with COVID-19, recent data suggest RAAS inhibitors do not increase plasma ACE2 concentrations.21 Ongoing randomized clinical trials will address whether RAAS inhibition has an effect on outcomes. Until such data are available, these agents should not be altered empirically.
Biomarkers of Comorbidity
Circulating markers of inflammation such as interleukin-6 (IL-6), C-reactive protein (CRP), and tumor necrosis factor have been consistently linked with heart failure and have even been associated with an increased risk of mortality.22-24 Unsurprisingly, in the massive proinflammatory, prothrombotic, cytokine storm mounted from critical illness related to SARS-CoV-2 infection, many biomarkers of comorbidity such as of IL-6, CRP, ferritin, and D-dimer are elevated,1 and at present there are early and ongoing studies aimed at neutralizing IL-6.25 Much in line with cardiac biomarkers, elevations in these non-specific markers of inflammation have prognostic value for patients with COVID-19, but do not necessarily indicate a treatment imperative.
Myocardial Remodeling
Biomarkers of myocardial remodeling such as soluble ST2 and galectin-3 are prognostic in heart failure,11,12 as are several matrix metalloproteases, tissue inhibitor of metalloproteinases1, collagen propeptides, myostatin, syndecan-4, N-terminal collagen III peptide, and osteopontin.11 To date, none of these biomarkers have been carefully studied in COVID-19 and little is known about their significance.
Interpretation of Heart Failure Biomarkers in the Context of COVID-19
COVID-19 is a systemic infection marked by inflammation, multi-organ involvement and evidence for cardiac stress and injury. Numerous biomarkers may be abnormal in patients with COVID-19, including inflammatory, hematologic, thrombotic and cardiac markers. Abnormalities of NT-proBNP and hs-cTn do not necessarily reflect heart failure or acute myocardial infarction. Marked elevation or rise in either marker may support clinical judgment regarding involvement of the cardiovascular system and prognosis in general. This can be used to support decision making regarding triage and subsequent management, including the use of cardiac imaging, physical exam encounters, and cardiologist collaboration.
Crucially important when measuring these biomarkers is to understand the goal of why they are being ordered and how their results might influence clinical care. Low concentrations of BNP/NT-proBNP or hs-cTn might help to triage patients away from imaging with echocardiography or computed tomography. On the other hand, in select patients with elevated or rising values of these biomarkers, a limited course of serial monitoring may prove useful. For example, such trajectory of change might identify a patient in whom a thoughtful imaging strategy might be employed, such as point-of-care ultrasound. When contemplating more extensive or invasive procedures, clinicians must balance risk of staff exposures and decontamination complexities with the potential benefits of more extensive/invasive testing.
In the excitement and uncertainty surrounding COVID-19 and cardiac biomarkers, we must remember that the inflammatory milieu is heightened, multiple organs are injured, and critical illness is often present. Because of this, the waters are muddy. With and understanding of the caveats mentioned above, together with clinical judgement, interpretation of abnormal cardiac biomarkers will more often become clear.
References
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62.
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020;Mar 27 [Epub ahead of print].
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802-10.
- Liu PP, Blet A, Smyth D, Li H. The science underlying COVID-19: implications for the cardiovascular system. Circulation 2020;142:68-78.
- Shi Y, Wang Y, Shao C, et al. COVID-19 infection: the perspectives on immune responses. Cell Death Differ 2020;27:1451–4.
- Loghin C, Chauhan S, Lawless SM. Pseudo acute myocardial infarction in a young COVID-19 patient. JACC Case Rep 2020-2:1284-8.
- Dabbagh MF, Aurora L, D'Souza P, Weinmann AJ, Bhargava P, Basir MB. Cardiac tamponade secondary to COVID-19. JACC Case Rep 2020;2:1326-30.
- Sala S, Peretto G, Gramegna M, et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J 2020;41:1861–2.
- Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020;323:1574–81.
- Hariri L, Hardin CC. Covid-19, angiogenesis, and ARDS endotypes. N Engl J Med 2020;May 21 [Epub ahead of print].
- Ibrahim NE, Januzzi JL Jr. Established and emerging roles of biomarkers in heart failure. Circ Res 2018;123:614–29.
- Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2017;70:776–803.
- Han H, Xie L, Liu R, et al. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J Med Virol 2020;92:819-23.
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:1-8.
- Bajwa EK, Boyce PD, Januzzi JL, Gong MN, Thompson BT, Christiani DC. Biomarker evidence of myocardial cell injury is associated with mortality in acute respiratory distress syndrome. Crit Care Med 2007;35:2484–90.
- Bajwa EK, Januzzi JL, Gong MN, Thompson BT, Christiani DC. Prognostic value of plasma N-terminal probrain natriuretic peptide levels in the acute respiratory distress syndrome. Crit Care Med 2008;36:2322–7.
- Metkus TS, Guallar E, Sokoll L, et al. Prevalence and prognostic association of circulating troponin in the acute respiratory distress syndrome. Crit Care Med 2017;45:1709–17.
- Benedict CR, Shelton B, Johnstone DE, et al. Prognostic significance of plasma norepinephrine in patients with asymptomatic left ventricular dysfunction. Circulation 1996;94:690–7.
- Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N Engl J Med 2020;382:1653–9.
- Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020;162:1671-81.
- Sama IE, Ravera A, Santema BT, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin–angiotensin–aldosterone inhibitors. Eur Heart J 2020;41:1810–7.
- Januzzi JL, Rehman S, Mueller T, van Kimmenade RRJ, Lloyd-Jones DM. Importance of biomarkers for long-term mortality prediction in acutely dyspneic patients. Clin Chem 2010;56:1814–21.
- Rauchhaus M, Doehner W, Francis DP, et al. Plasma cytokine parameters and mortality in patients with chronic heart failure. Circulation 2000;102:3060–7.
- Anand IS, Latini R, Florea VG, et al. C-Reactive protein in heart failure: prognostic value and the effect of valsartan. Circulation 2005;112:1428–34.
- Xu X, Han M, Li T, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A 2020;117:10970–5.
Clinical Topics: Anticoagulation Management, COVID-19 Hub, Heart Failure and Cardiomyopathies, Pericardial Disease, Acute Heart Failure, Heart Failure and Cardiac Biomarkers
Keywords: Heart Failure, COVID-19, Coronavirus, severe acute respiratory syndrome coronavirus 2, SARS Virus, Pandemics, Interleukin-6, Syndecan-4, Cardiovascular Diseases, Peptidyl-Dipeptidase A, C-Reactive Protein, Galectin 3, Norepinephrine, Osteopontin, Angiotensin-Converting Enzyme Inhibitors, Prognosis, Renin-Angiotensin System, Critical Illness, Hospital Mortality, Natriuretic Peptide, Brain, Coronavirus Infections, Peptide Fragments, Disease Progression, Prognosis, Biomarkers, Pharmacological, Biomarkers, Respiratory Distress Syndrome, Takotsubo Cardiomyopathy, Oxygen, Patient Discharge, Cardiac Tamponade
< Back to Listings