Feature Story | Real-World Evidence: Perceptions of Cardiologists

Real-time data registries, like those in ACC’s NCDR, collect real-time patient data on specific cardiac conditions. Such registries are continually updated with real-time data on patients and their conditions, therapy and outcomes, providing “a comprehensive snapshot of the actual care and outcomes associated with a particular condition,” according to Thomas M. Maddox, MD, MSc, FACC. The real-world evidence (RWE) generated by registries and other data sources are often used by cardiologists along with randomized clinical trial (RCT) data to make treatment decisions.
An ACC survey of 173 U.S. cardiologists conducted in July 2017 found a clear split on the value of RWE and different tools for patient treatment decisions. Among several clinical tools listed, 71 percent of those surveyed said that clinical practice guidelines are either the most important or second most important tool, followed by clinical trials (43 percent) and appropriate use criteria (24 percent), whereas only 16 percent listed RWE as the most important.
"Real-world evidence is an important tool in our arsenal of evidence supporting the care we provide. The survey results indicate that cardiologists are using them, in conjunction with RCTs and other sources of evidence, to inform their care decisions." — Thomas M. Maddox, MD, MSc, FACC
“The response is not surprising and is appropriate. Guidelines, which are based on the body of evidence for treatments, provide a perspective on optimal patient care. Registries provide a perspective on the extent to which guideline recommendations are adopted in practice,” says Frederick A. Masoudi, MD, MSPH, FACC, chair of the NCDR Management Board and NCDR chief science officer.
Maddox, however, was surprised to see the low confidence in health system protocols for clinical treatment decisions, which only 4 percent of respondents ranked as the most or second most important tool. “Health system protocols, done well, can markedly improve both the clinical outcomes and the value associated with care delivery. So, I think digging into these results and working to improve any deficiencies in health system protocols is important,” he says.
Interestingly, mid-career cardiologists (21 percent) and late career cardiologists (15 percent) were more likely to be extremely familiar with RWE than early career cardiologists (4 percent). Among cardiologists familiar with RWE, 30 percent were very/extremely confident in RWE findings, while 11 percent were not confident and 23 percent said their confidence depends upon the research itself. “I have noticed very disparate results from RWE on the same topics that could be confusing!” one respondent wrote.
Cardiologists familiar with RWE were also divided on how often they apply RWE learnings into practice. Whereas 23 percent indicated they always or often applied the learnings they gather from RWE into practice, 21 percent said they rarely or never applied RWE learnings into practice. Nearly half (48 percent) sometimes applied RWE learnings in their practices.
The survey also asked about familiarity with the Dabi-Riva study, which analyzed Medicare beneficiary claims data for over 100,000 patients 65 years or older with nonvalvular atrial fibrillation (AFib) and explored intracranial and major extracranial bleeding events given patient usage of rivaroxaban or dabigatran. Among cardiologists familiar with RWE, 56 percent were not familiar with the Dabi-Riva study, while 43 percent said they were. The majority of cardiologists (58 percent) who were aware of the Dabi-Riva results were likely to incorporate the findings into their treatment regimen for patients with nonvalvular AFib.
When queried about the relative usefulness of RWE and RCT data, 89 percent of those familiar with RWE responded that RWE and RCT data can provide useful guidance for clinical decision making. However, 61 percent of respondents said RCT results are more valid for clinical decision making compared with RWE. Almost as many (58 percent) agreed that RWE allows clinicians to tailor health care decisions more closely to individual patient characteristics, while 57 percent said RWE enables more effective clinical assessments and decision making over a broader patient population.
Approximately half (51 percent) of respondents said RCTs are not focused enough on real-world patients. “RWE is probably useful to identify gaps in appropriate use between RCTs and the real world,” commented one respondent. Interestingly, cardiologists were more evenly divided as to whether RWE inappropriately supersedes the traditional paradigm in which authoritative medical evidence is generated through RCTs, validated through peer-reviewed publication in reputable journals and incorporated into broadly applied clinical practice guidelines, with 36 percent in agreement and 28 percent not in agreement.
“RCTs – which provide the foundation for most of our clinical practice guidelines – remain the ‘gold standard’ for understanding the specific impact of a therapy on a particular condition. However, many patients differ significantly from those participating in trials, so being able to supplement our knowledge with RWE is helpful,” says Maddox.
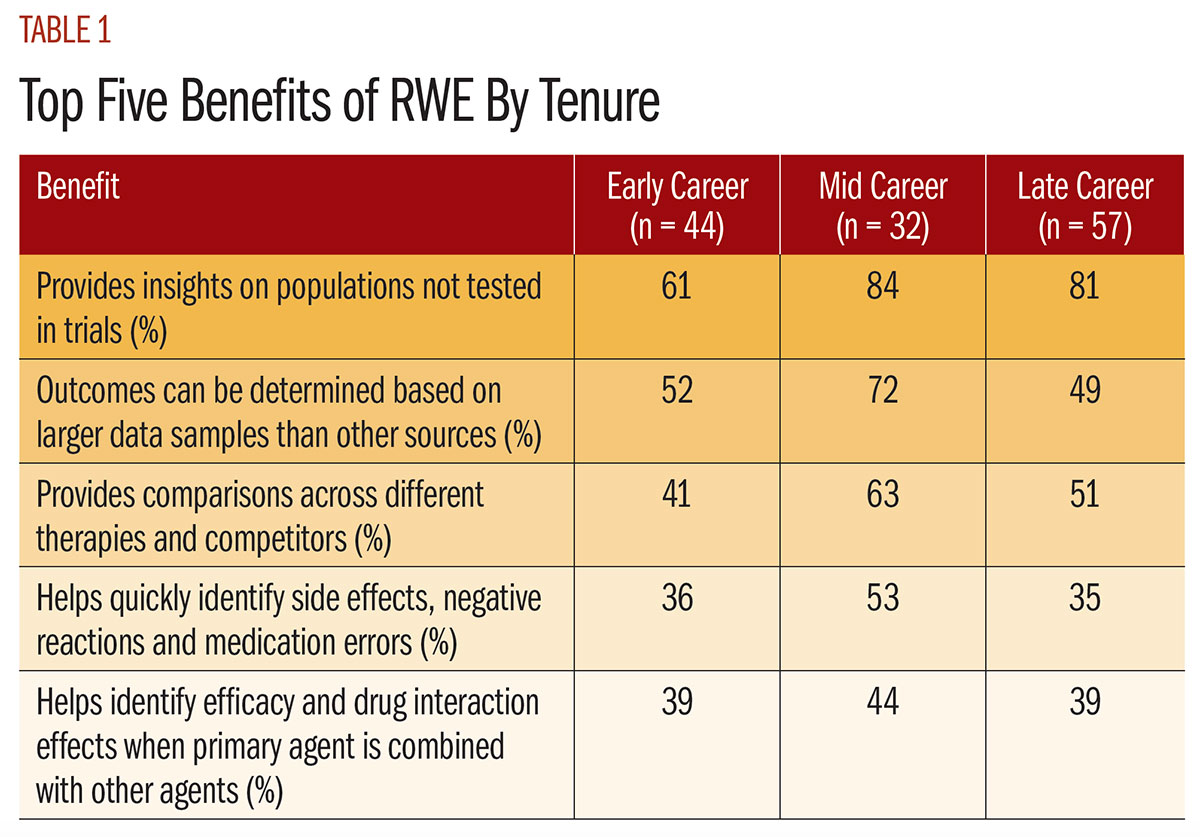
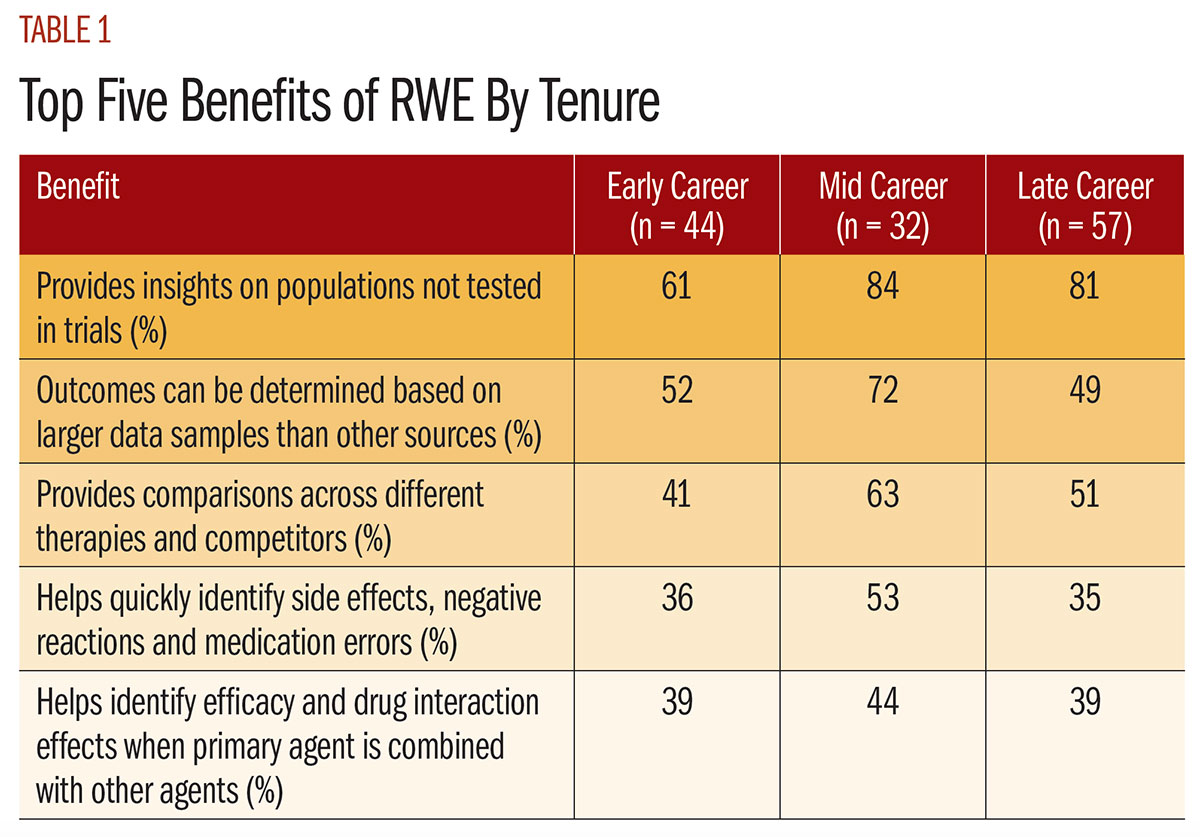
More than nine out of 10 cardiologists familiar with RWE (94 percent) identified at least one benefit of using RWE. The top benefit, selected by 75 percent, was that RWE provides insights on populations not tested in trials. More than half of the respondents also noted that outcomes can be determined based on much larger data samples than other sources (56 percent) and that RWE provides comparisons across different therapies and competitors (50 percent). The top five benefits of RWE as viewed by career tenure are detailed in Table 1.
“RWE is an important tool in our arsenal of evidence supporting the care we provide. The survey results indicate that cardiologists are using them, in conjunction with RCTs and other sources of evidence, to inform their care decisions,” Maddox says.
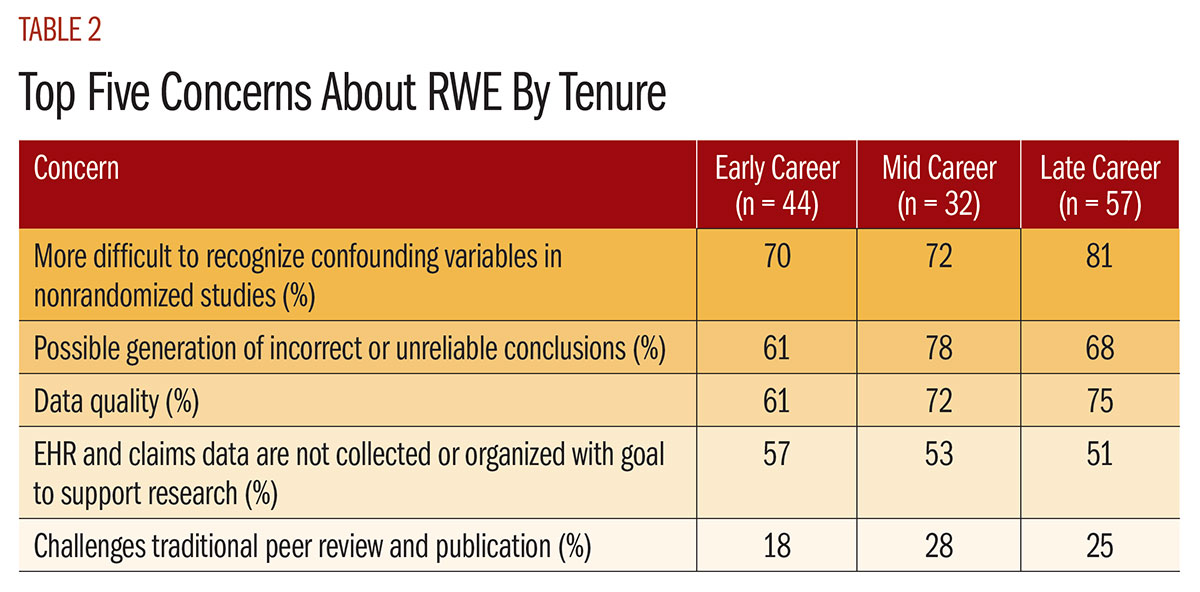
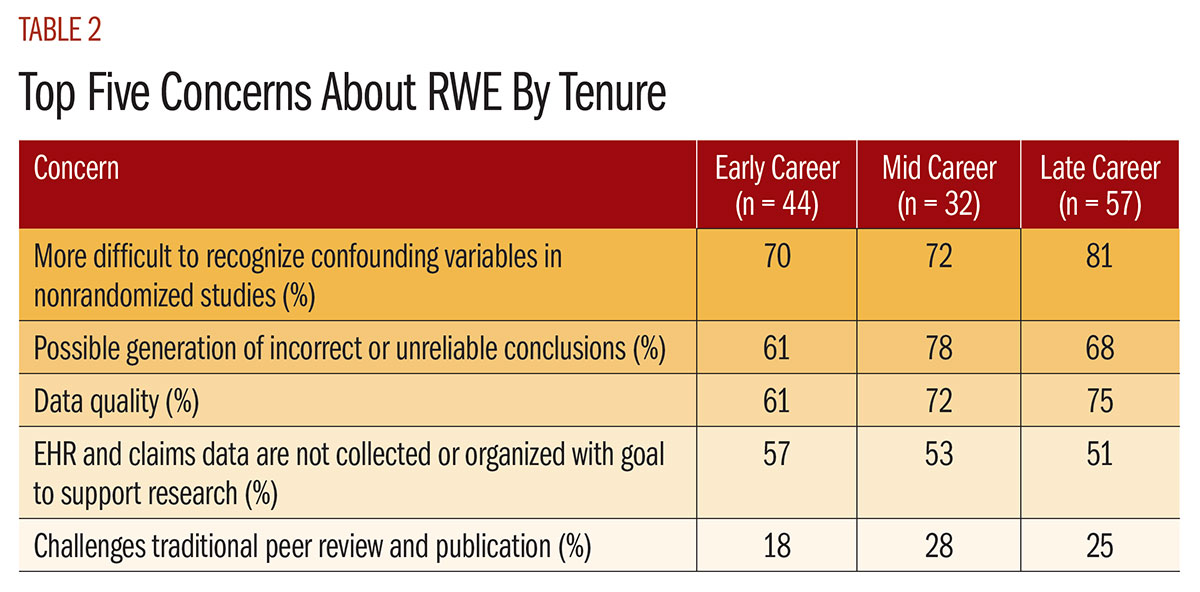
Similarly 94 percent of those surveyed identified at least one concern with RWE, with the top three concerns being: 1) difficulty recognizing confounding variables in nonrandomized studies (73 percent); 2) possible generation of incorrect or unreliable conclusions (70 percent); and 3) data quality (69 percent). Additionally, 52 percent of respondents noted that EHRs and claims data are not collected or organized with the goal of supporting research. Table 2 details the top five concerns about RWE as viewed by career tenure.
“I share my colleagues’ concerns about teasing out true treatment effects from inherent biases present in real-world practice,” says Maddox. “That’s why pairing RWE with RCTs, where possible, is so essential.”
More than three out of five cardiologists familiar with RWE (61 percent) were very/extremely confident in registry data as an RWE source. However, less than three out of 10 were very/extremely confident in EHRs (29 percent), pharmacy data (28 percent) and clinician notes (26 percent). Even fewer were very/extremely confident in administrative claims data (17 percent), patient forums (8 percent) and social media (3 percent). “EHRs, clinician notes and administrative claims are not good sources as often providers are entering what is easy for them, not what is accurate, due to inadequacies and time constraints with EHRs,” wrote one respondent.
According to Maddox, this certainly fits with [his] experience in studying EHR data via the NCDR PINNACLE registry, but we have to do better. He adds, “The potential of EHRs in generating robust clinical data for RWE is huge, but we need better work from our EHR colleagues in designing better user interfaces and data collection methods to effectively and efficiently capture our clinical care.”
Meanwhile, the majority of cardiologists at all tenure levels (64 percent) said they were very/extremely interested in ACC education regarding RWE. One respondent wrote, “If real-world experience is coming, it is in the interest of the cardiology community to become better educated. The ACC can use its existing publications and electronic media to inform its members.” According to Masoudi, the ACC has several sources of education materials that touch on the use of data in clinical care. He cautions that it is important to recognize the strengths and limitations of various data sources.
"Guidelines, which are based on the body of evidence for treatments, provide a perspective on optimal patient care. Registries provide a perspective on the extent to which guideline recommendations are adopted in practice." — Frederick A. Masoudi, MD, MSPH, FACC
Maddox points out the NCDR has some of the largest and most advanced cardiovascular real-time registries in the world, which have generated hundreds of RWE studies to better inform clinical decision making. “The investigators involved in these studies often go to great lengths to inform the reader about their limitations, so careful reading of these works is an important piece of education about RWE,” he says. Additionally, published clinical reviews and in-person education sessions on RWE are periodically offered by the ACC. “More can always be done, but I think the survey results indicate that the cardiology community is appropriately educated about the benefits and limitations of RWE. This suggests that RWE education efforts – be they provided by ACC or others – are having an impact,” says Maddox.
Those surveyed who said they always or often apply RWE findings all indicated that RWE and RCT data can provide useful guidance for clinical decision making (100 percent); that RWE enables more effective clinical assessments and decision making over a broader patient population (85 percent); and that RWE allows them to tailor health care decisions more closely to the characteristics of an individual patient (79 percent). Not surprisingly, they were also more likely to have strong overall confidence in the findings from RWE research either overall (62 percent) or specific to a particular set of RWE findings (26 percent). Additionally, they were more likely to have confidence in registry data as an RWE source (71 percent) and were likely to have confidence in EHRs as an RWE data source (56 percent).
Masoudi believes the strengths and limitations of observational analyses should be taken into account in the interpretation of RWE findings. “The issue of confounding should always be considered. Relationships identified with observational data should be identified as associations rather than clearly causal relationships,” he notes. “We’ll never be done learning in cardiology and medicine, so striving to always improve our evidence base is essential. I view RWE as a critical tool in that effort, and was pleased to see that my colleagues believe so too,” concludes Maddox.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Cardiovascular Care Team, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: ACC Publications, Cardiology Magazine, ACC18, ACC Annual Scientific Session, Atrial Fibrillation, Decision Making, Clinical Protocols, Confounding Factors, Epidemiologic, Antithrombins, Decision Making, Goals, Information Storage and Retrieval, Medicare, Patient Care, Pharmaceutical Services, Pharmacies, Pharmacies, Pharmacy, Publications, Reading, Registries, Research, Research Personnel, Social Media, Health Care Surveys, Touch
< Back to Listings