Special Section | The Evolution of the Physician Assistant Workforce in Cardiology
This article is adapted from a manuscript by the Writing Committee of ACC’s PA Work Group. The Writing Committee Members are pictured left to right below. They acknowledge the assistance of Kelli Bohannon and Abby Cestoni.
 Dorothy D. Pearson, BA, PA-C, AACC (chair)
Dorothy D. Pearson, BA, PA-C, AACC (chair)
 Sondra M. DePalma, MHS, PA-C, AACC
Sondra M. DePalma, MHS, PA-C, AACC
 Sharon M. Dickinson, MS, PA-C, AACC
Sharon M. Dickinson, MS, PA-C, AACC
 Camille J. Dyer, MS, PA-C, AACC, DFAAPA
Camille J. Dyer, MS, PA-C, AACC, DFAAPA
 Viet T. Le, MPAS, PA-C
Viet T. Le, MPAS, PA-C
 KellyAnn Light-McGroary, MD
KellyAnn Light-McGroary, MD
 Sherrie R. Webb, BS, PA-C
Sherrie R. Webb, BS, PA-C
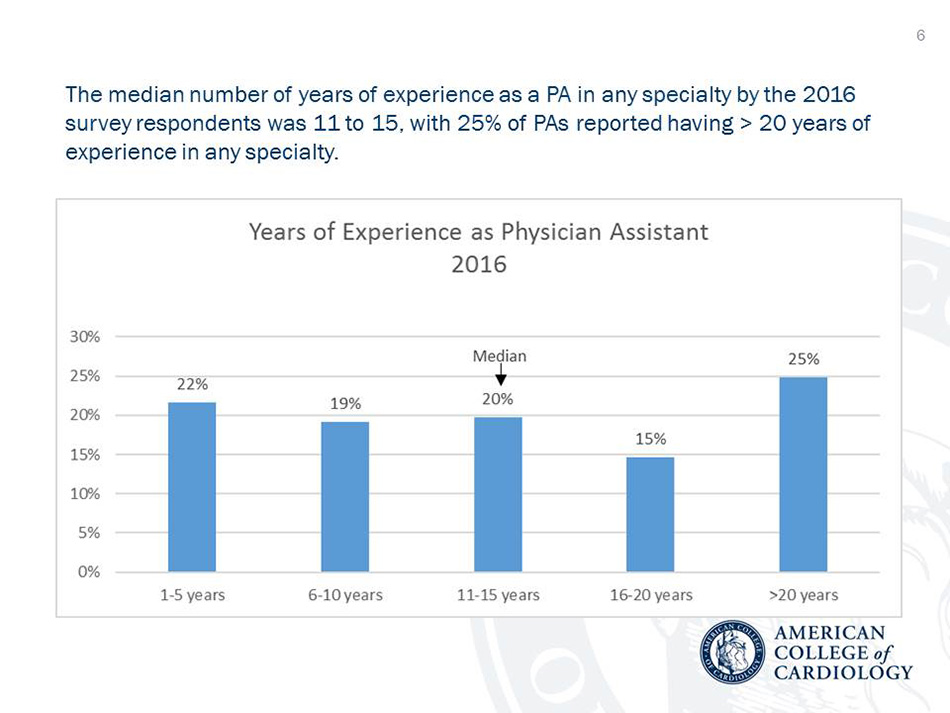
Physician assistants (PAs) are health care professionals who are helping to address the growing need for high-quality cardiovascular health care providers in the U.S. As the PA profession marks its 50th anniversary, a new survey reveals that as the profession has matured, so has the role of PAs who work in cardiology. Conducted by the ACC’s PA Work Group of the Cardiovascular Team Council, the survey provides important insights into the experience, scope of practice and services provided in cardiovascular practice, as well as opportunities to enhance professional membership. More work experience in cardiology and greater autonomy in providing cardiovascular care are two notable findings among the current generation of PAs.
The disparity continues between supply of cardiovascular specialists and demand for cardiovascular care.1,2 An estimated 22,000 cardiologists practice in the U.S.3 A deficit of 7,080 FTEs is projected by the HRSA: Health Workforce Analysis to meet a projected 20 percent increase in demand in 2025. About 3,300 PAs report working in cardiology in 2016, according to National Commission on Certification of Physician Assistants (NCCPA) data,4 representing a substantial addition to the workforce.
ACC is a strong proponent of team-based care to improve access to health care, improve health care efficiency, increase productivity, improve care coordination and supplement physician-provided care in cardiology.1,4 In 2009, the College first identified the opportunity for increased utilization of PAs and other advanced practice providers (APPs) and recommended increased training and development of best practices for team-based care.1 Its commitment was supported by the publication of the 2015 ACC Health Policy Statement on Cardiovascular Team-Based Care and the Role of Advanced Practice Providers,5 which stated “cardiovascular team-based care is a paradigm for practice that can transform care, improve heart health, and help meet the demands of the future.”
The Survey Says!
The response rate for the PA Workforce survey, conducted electronically in 2016, was 10.4 percent (363 of 3,501 PAs working in cardiology). Forty-six percent of respondents were ACC members. The results were compared with those from 340 PAs surveyed in 2012.5
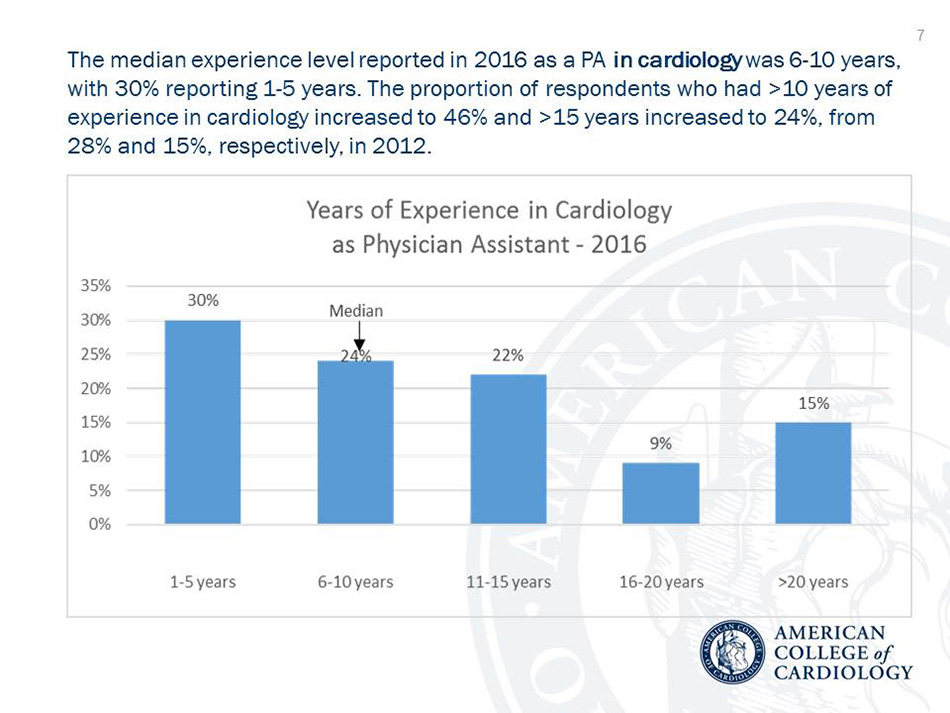
The median work experience as a PA in cardiology was six to 10 years as reported by 24 percent; 30 percent reported one to five years. Further, the proportion of respondents who had >10 years of experience in cardiology increased to 46 percent and >15 years increased to 24 percent, from 28 percent and 15 percent, respectively, in 2012.
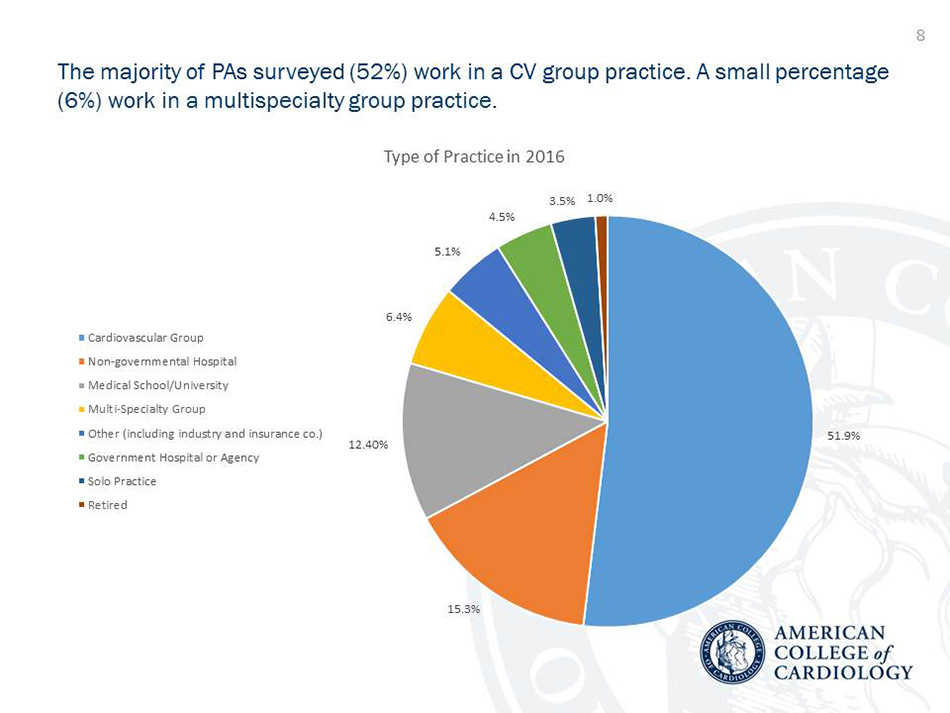
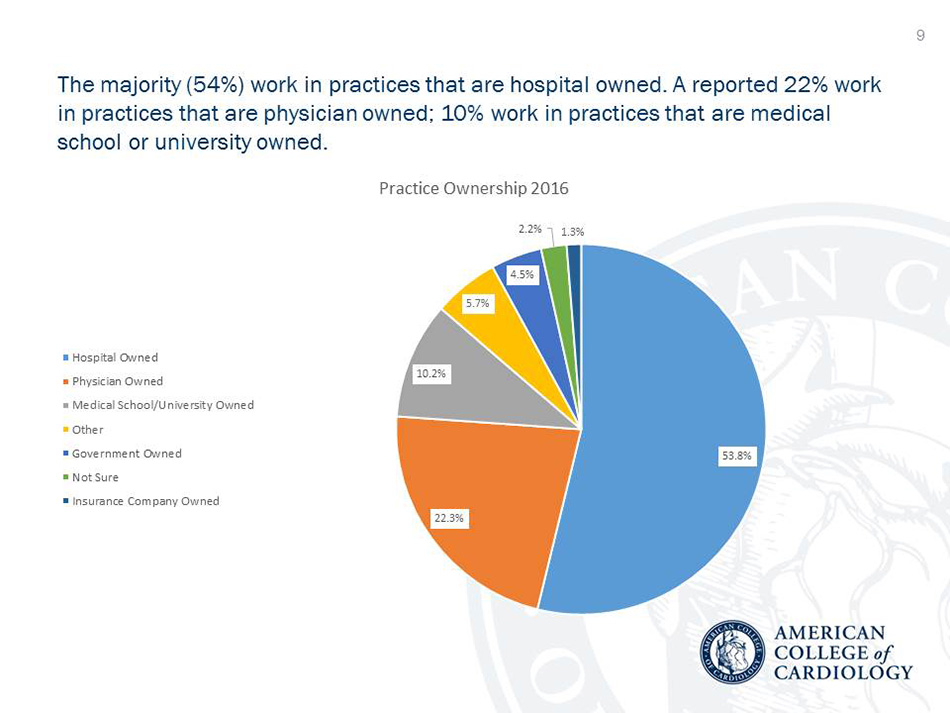
The most common work setting was a cardiovascular group practice (52 percent), then non-governmental hospital (15 percent), medical school/university (12 percent) and multispecialty group (6 percent). For most PAs (54 percent), the practice was hospital owned, and physician owned for 22 percent and medical school or university owned for 10 percent. A work week of ≥ 35 hours was reported by >88 percent of PAs.
The locale for their work was urban for 57 percent, suburban for 48 percent and rural for 14 percent (some reported working in multiple locations). In the 2012 survey, 48 percent and 53 percent worked in urban and suburban settings, respectively, and 15 percent reported working in a rural setting.
The majority (67 percent) of cardiology PAs had both inpatient and outpatient responsibilities, compared with 77 percent in 2012. However, compared with the 2012 survey, there was a trend for more PAs to report only inpatient (11.5 vs. 18 percent) or outpatient (11.5 vs. 15 percent) duties. The median number of patients treated by a PA each week was 26-50 in either the inpatient or outpatient setting (potentially >50-100 for combined responsibilities).
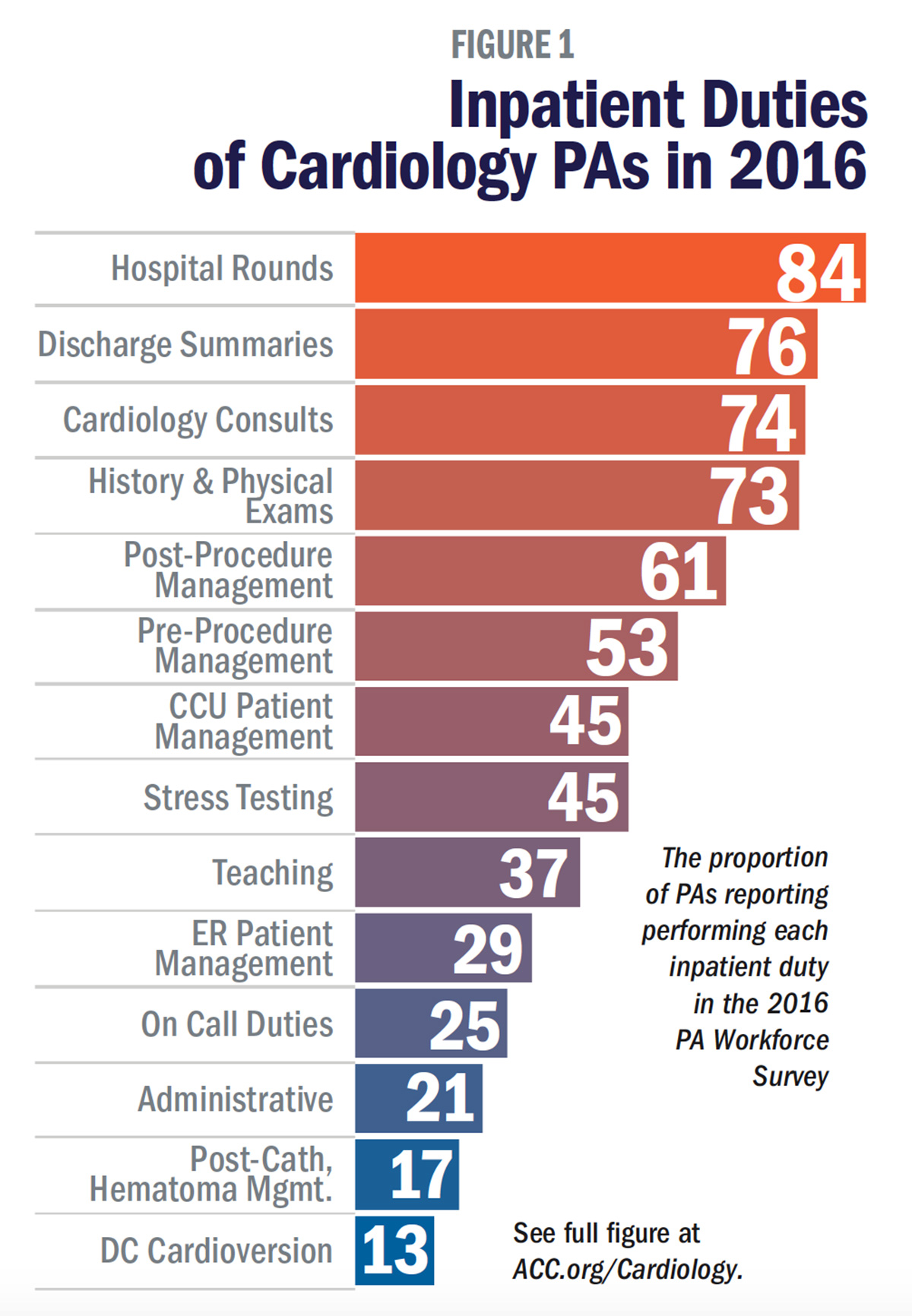
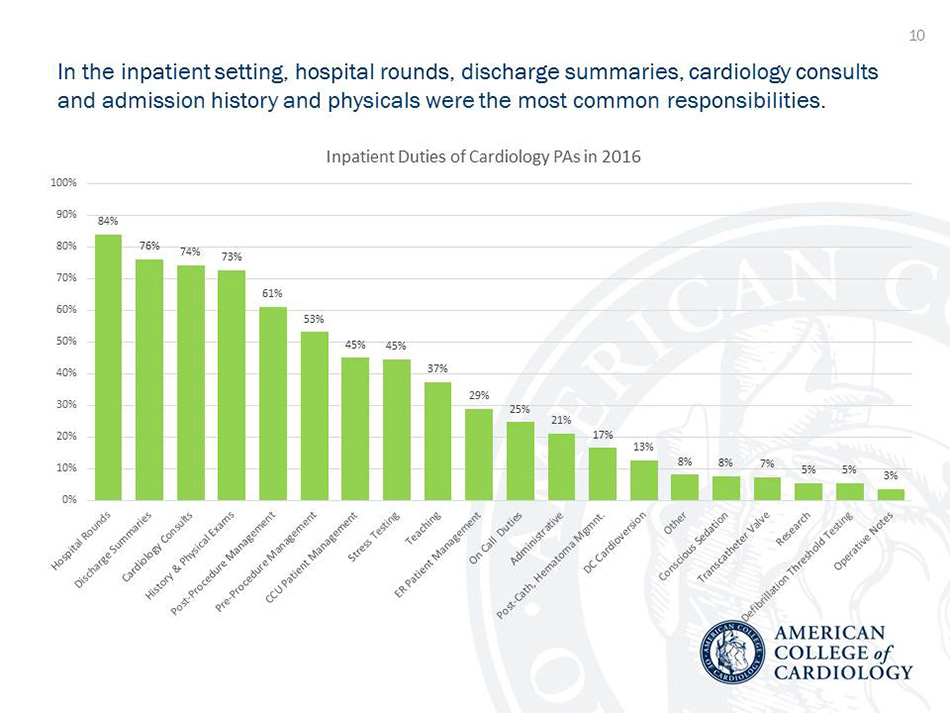
In the inpatient setting, hospital rounds, discharge summaries, cardiology consults and admission history and physicals were the most common responsibilities (Figure 1). Compared with the 2012 survey results, statistically significant differences were found for four areas of responsibility. Fewer PAs reported performing admission history and physicals (82 vs. 73 percent), patient management responsibilities in the emergency department (ED) (41 vs. 29 percent) and inpatient research responsibilities (16 vs. 5 percent). In contrast, more PAs in 2016 reported post-procedure management responsibilities (61 percent vs. 50 percent in 2012).
The reasons for the reduction in admission history and physicals and ED responsibilities are unclear, but may reflect a trend towards consult-only cardiology practice, rather than one that receives many admissions from the ED. Hospitalist services may be handling a higher volume of ED admissions for chest pain and other cardiac diagnoses.
The increase in post-procedure management by PAs may be due to several factors, including: 1) overall increased acceptance and utilization of APPs using a team-based approach to cardiac care; 2) emphasis on efficiency in care delivery, promoting top of license responsibility for APPs; 3) relative scarcity of cardiologists in some settings; 4) introduction of new and sometimes complex cardiac procedures, such as transcatheter aortic valve replacement and left atrial appendage occlusion device implant; and 5) broadened indications for and increased volume of certain procedures, such as for ICDs (including subcutaneous) and electrophysiologic ablation procedures.
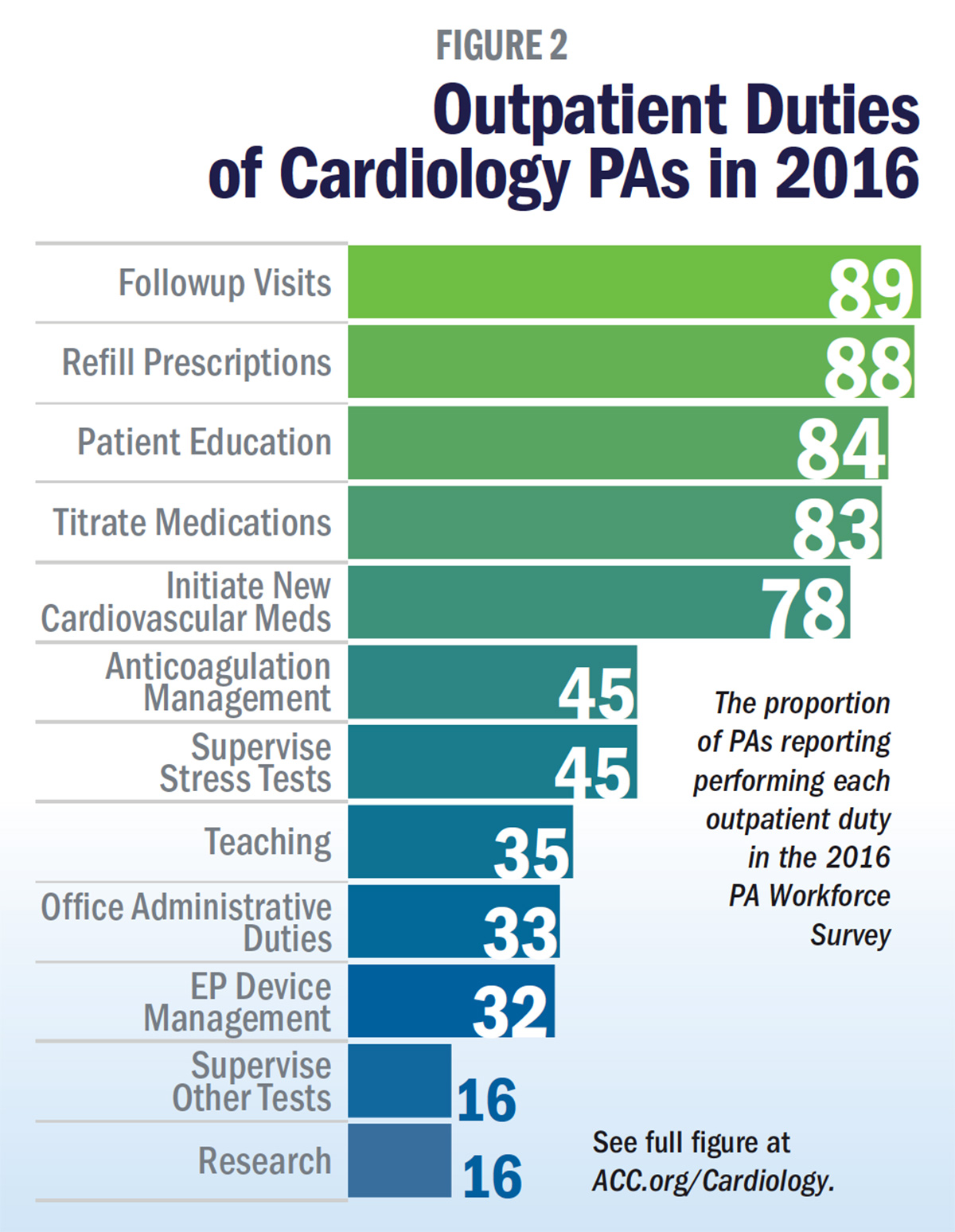
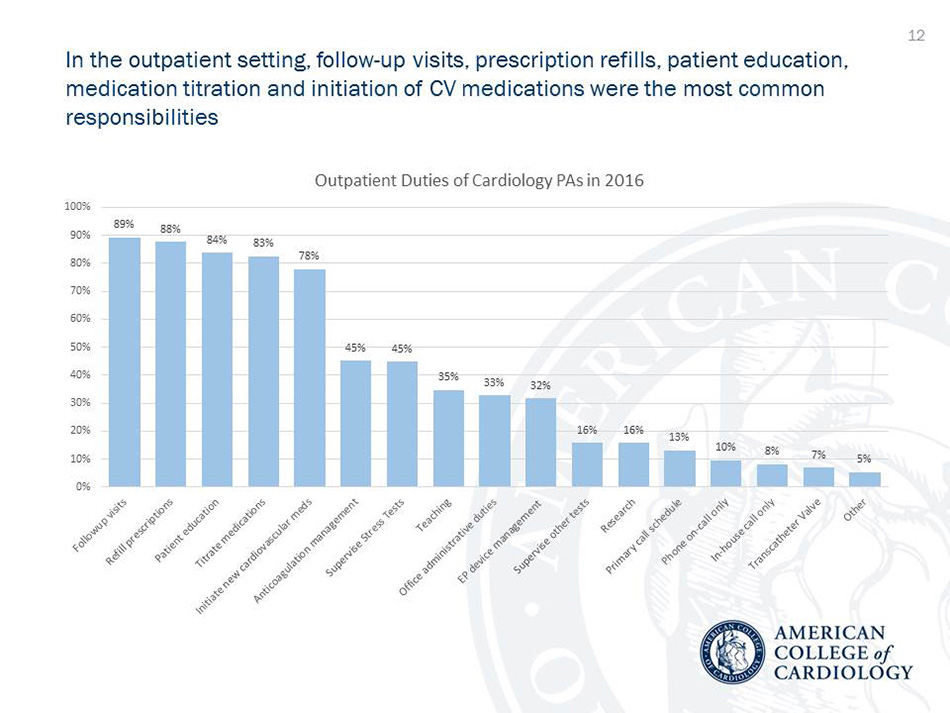
In the outpatient setting, follow-up visits, prescription refills, patient education, medication titration and initiation of cardiovascular medications were the most common responsibilities (Figure 2). Compared with 2012 results, significantly fewer PAs reported supervising stress tests (55 vs. 45 percent) or other tests (23 vs. 16 percent). Most PAs indicated that supervision and reimbursement guidelines for cardiac stress testing were not a concern in their practice.
The reported decrease in test supervision could reflect a shift towards more testing being conducted in a facility vs. office setting. It also could reflect a trend for stress test supervision to be performed increasingly by nurses or other trained personnel (rather than by PAs or nurse practitioners), with general supervision provided by an onsite cardiologist. Indeed, a scientific statement on the supervision of exercise testing, issued in 2014 by the American Heart Association, concluded that “in most cases, clinical exercise tests can be safely supervised by properly trained non-physician health professionals” meeting specified criteria.
Another notable decrease in the 2016 survey was in the proportion of PAs who had research responsibilities in either the inpatient (significant vs. 2012) or outpatient setting. Although the reasons for this shift are not known, one factor may be increased salaries for PAs, especially if similar responsibilities could be performed by nurses or other professionals.
Clinical autonomy for cardiology PAs increased in 2016 compared with 2012. The majority (65 percent) of PAs reported they work with an attending cardiologist who is onsite most of the time and available for consultation. Only 16 percent reported that most of their duties require interaction with the attending cardiologist (down from 22 percent in 2012) – and 19.5 percent reported they practice while an attending is offsite but available for immediate consultation (up from 13.5 percent in 2012).
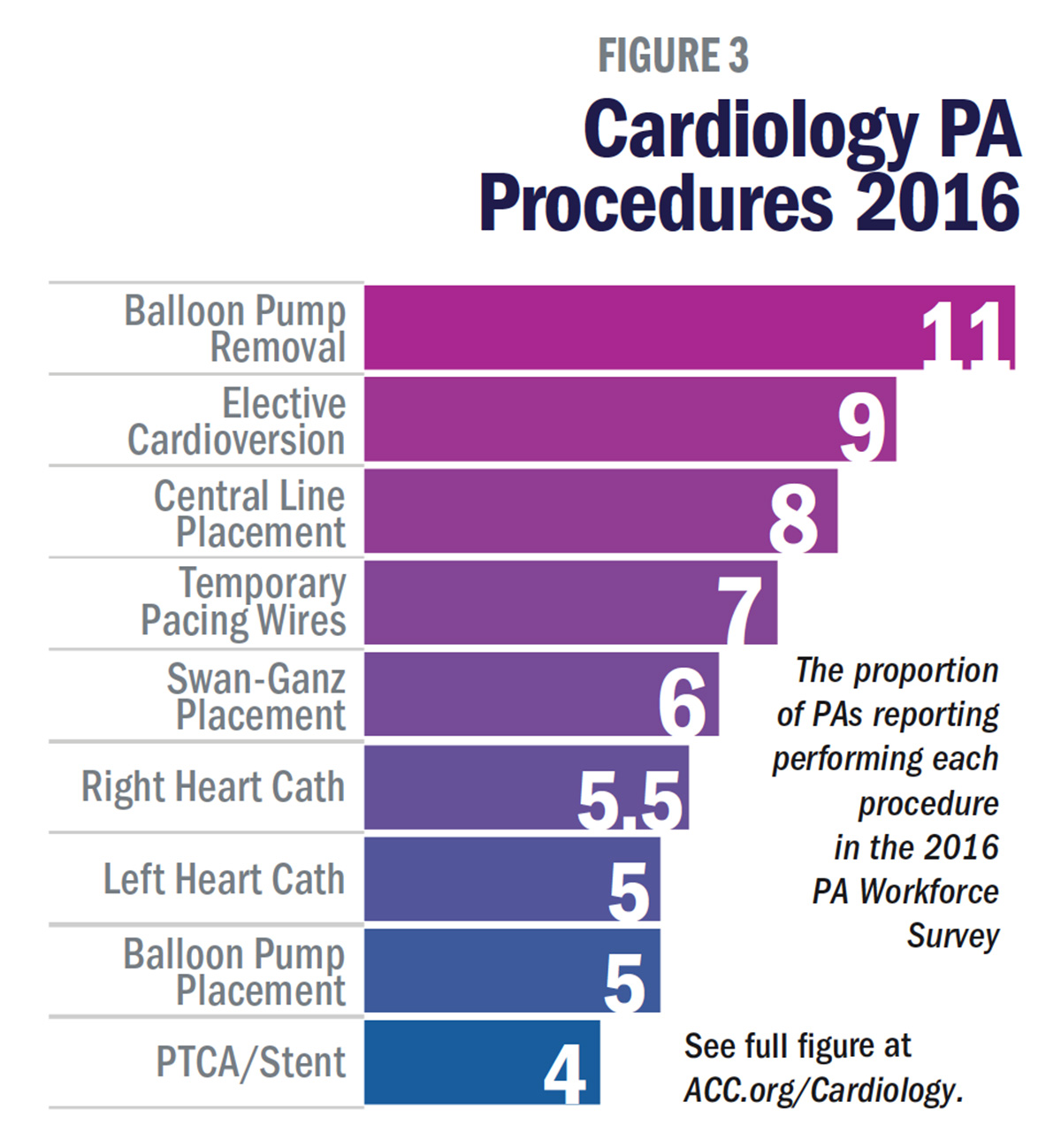
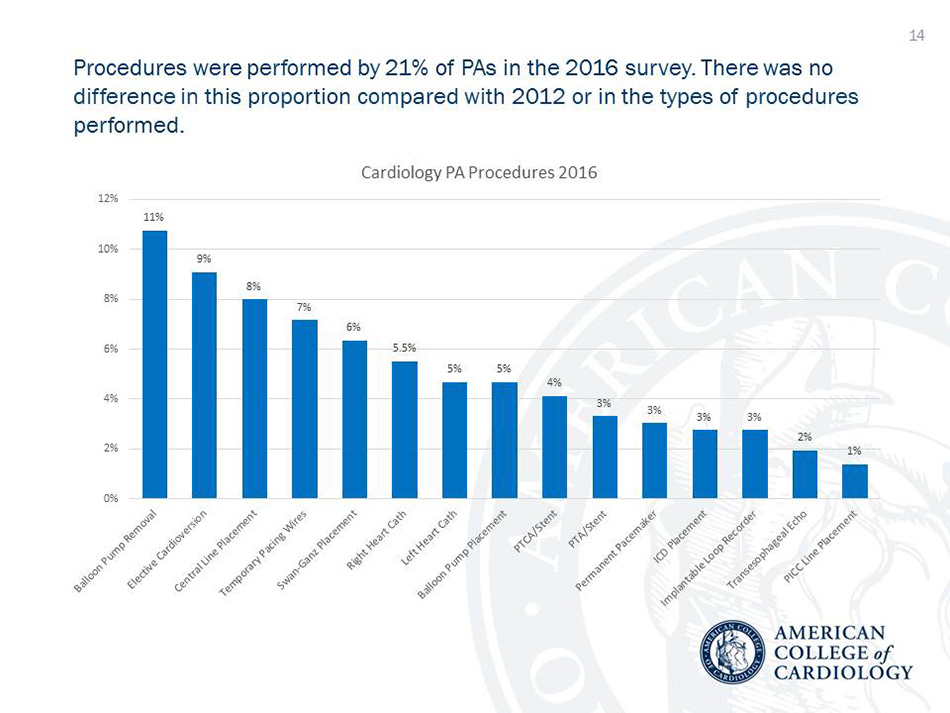
Procedures were performed by 21 percent of PAs in the 2016 survey. There was no difference in this proportion compared with 2012 or in the types of procedures performed. The types of procedures and the proportion of PAs performing them are shown in Figure 3. Here again, more autonomy for the PA was found, with 46 percent performing procedures in a setting where the attending cardiologist was onsite but not necessarily in the procedure room, compared with 36 percent in 2012 – and 16 percent performed procedures when the attending was offsite but accessible if needed, up from 8 percent in 2012. Fewer PAs reported the attending cardiologist usually participated in the procedure, only 21 percent, down from 39 percent.
Increased acceptance of PAs by hospitals, insurers and patients, along with a relatively short supply of cardiologists and a desire by physicians for a favorable work-life balance may all contribute to greater autonomy for PAs. Higher levels of autonomy when performing procedures may be impacted by the same factors affecting overall clinical autonomy. However, the most critical factor is likely hospital credentialing processes. The ability to perform any procedure requires appropriate training, demonstration of competence and appropriate hospital credentialing. Some hospitals may have revised their credentialing processes for APPs in recent years.
In addition, some hospitals may be employing PAs (as well as nurse practitioners) to work exclusively in coronary and/or critical care units; performance of critical care procedures may be a normal and expected part of the PA’s job responsibility. Hospitals and/or the medical staff may be establishing defined training tracks for the mastery of such procedures in this setting.
A minority of PAs reported performing invasive cardiac catheterization, pacemaker and ICD procedures. The autonomy level when performing these procedures is not known. A few PAs in academic settings may be functioning in a role ordinarily reserved for a cardiology fellow, with similar if not equivalent training opportunities. Other PAs in the cardiac catheterization laboratory may be functioning as an assistant to the attending cardiologist.
Training and Professional Membership
PAs are nationally certified and state-licensed medical professionals. They are educated in a master’s degree program lasting two to three years that is modeled on the medical school curriculum, including didactic courses and more than 2,000 hours of clinical rotations. Before entering a PA training program, students have a median of 100 weeks of health care experience. PA certification is granted by the NCCPA. Maintenance of certification requires completing 100 hours of continuing medical education every two years and passing a recertification exam every 10 years.
According to the 2016 survey, most PAs (88 percent) did not have any structured post-graduate training in cardiology or focused guidance to assist their evolution into the practice of cardiology. Of those who had training or assistance, required reading was reported by 58 percent, cardiology rotation by 55 percent, a formal training program by 29 percent and a formal residency program by 19 percent.
Notably, 51 percent reported they would seek specialty recognition if it was offered and 38 percent said they might seek this. Interest was expressed by 63 percent in an NCCPA Certificate of Added Qualification and by 59 percent in a designation based on years of experience in the specialty, as well as in online courses leading to recognition (58 percent), specialty continuing medical education requirements (49 percent) or specialty examination (43 percent).
Membership in ACC and the American Academy of Physician Assistants, although held by a majority, declined from 2012. For ACC, membership was held by 53 percent, down from 66 percent, and for American Academy of Physician Assistants it was 66 percent, down from 79 percent. Membership in the APAC was 16 percent in 2016, down from 22 percent, and membership in the American Heart Association eight percent, down from 12 percent. Declines in reimbursement allocation by practices for professional memberships may contribute to the reduction in membership in these organizations. Another factor may be the emergence of other organizations competing for membership dollars, including physician organizations that now welcome PAs, subspecialty organizations, and other PA organizations at the national, state or local level.
Of the respondents in 2016, 10 percent had received the designation of Associate of the American College of Cardiology (AACC); 22 percent planned to pursue this designation, 29 percent did not and 38 percent were unsure. At the time of the survey, 6 percent of respondents were currently serving on an ACC council, committee or task force, while 25 percent expressed interest in doing so in the future. Thirty-six percent of 306 respondents expressed interest in learning about volunteer opportunities with the ACC Physician Assistant Work Group.
The ACC is well positioned to serve as the professional home for PAs in cardiology, with its support of education, advocacy and an enhanced patient care experience. Within advocacy, the ACC has successfully worked with PA leaders in support of home health care legislation and other areas of mutual interest. Professional organizations such as the ACC can provide support in the development and promotion of professional PA competencies (in cardiology or other fields). Exploration of advanced cardiovascular education for cardiology PAs, perhaps mirrored in COCATS (ACC’s Core Cardiovascular Training Statement) may be warranted. Adoption of clinical ladders by health care systems for the career and professional development of cardiology APPs may be a further avenue for recruiting and retaining needed talent. The mutual interests of hospitals, physicians, patients and APPs are all served by promoting enhanced cardiovascular education and training for those working in the field.
References
- Rodgers GP, Conti JB, Feinstein JA, et al. J Am Coll Cardiol 2009;54:1195-6.
- Dall TM, Gallo PD, Chakrabarti R, et al. Health Affairs 2013;32:2013-20.
- Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025. Available at: www.aamc.org. Accessed Jan 11, 2018.
- National Commission on Certification of Physician Assistants. 2016 Statistical Profile of Certified Physician Assistants. Available here. Accessed Jan 9, 2018.
- Brush JE, Handberg EM, Biga C, et al. J Am Coll Cardiol 2015;65:2118-36.
- American College of Cardiology. Highlights of the ACC Physician Assistant Workforce Survey 2012. Available at: http://www.acc.org. Accessed Jan 5, 2018.
Clinical Topics: Cardiac Surgery, Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention
Keywords: ACC Publications, Cardiology Magazine, American Heart Association, Anniversaries and Special Events, Atrial Appendage, Cardiac Catheterization, Career Mobility, Certification, Chest Pain, Credentialing, Critical Care, Curriculum, Education, Medical, Continuing, Efficiency, Emergency Service, Hospital, Exercise Test, Fellowships and Scholarships, Fibrinogen, Follow-Up Studies, Group Practice, Health Policy, Health Services Accessibility, Hospitalists, Inpatients, Insurance Carriers, Internship and Residency, Medical Staff, Nurse Practitioners, Outpatients, Pacemaker, Artificial, Patient Care, Physician Assistants, Referral and Consultation, Salaries and Fringe Benefits, Schools, Medical, Specialization, Students, Transcatheter Aortic Valve Replacement, Work-Life Balance
< Back to Listings