Atrial Fibrillation, Atrial Tachycardia: What’s the Difference?
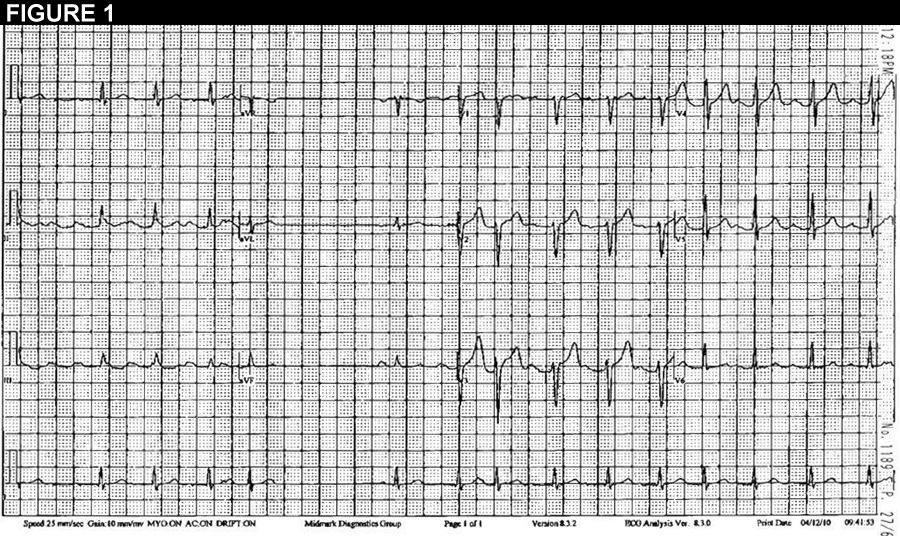
A 50-year old-male is referred to our electrophysiologic service for evaluation of palpitations. Prior Holter monitoring demonstrated episodes of atrial fibrillation as well as an atrial tachycardia. Further diagnostic testing included a 2D echocardiogram demonstrating evidence of globally depressed left ventricular (LV) function with an ejection fraction (EF) of 33%. The patient did not demonstrate signs or symptoms of heart failure, and regularly exercised. He underwent electrophysiologic study at an outside institution. This study noted “disorganized atrial activity with earliest activation in the left atrium consistent with atrial fibrillation/flutter.” Given the left sided location, the treating physicians decided to pursue medical management with beta blockers and a class Ic antiarrhythmic. He was interested in catheter ablation due to intolerance of medications, and was referred to our facility.
|
|
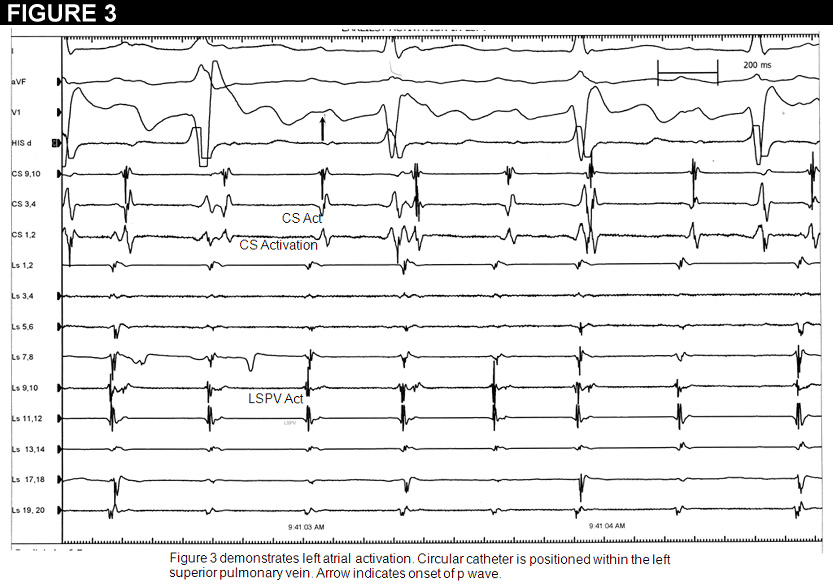
The patient was taken to the electrophysiologic laboratory. We performed electro-anatomic mapping in the right atrium with demonstration of late activation times. We then accessed the left atrium through a standard double trans-septal access. The circular catheter was then placed at the os of each pulmonary vein. The left superior pulmonary vein demonstrated the earliest potentials 40msec in advance of the surface p wave (Figure 3). We decided to ablate in this region, which was anatomically on the mid posterior wall of the left atrium at the os of the left superior pulmonary vein. Within several seconds of ablation, there was complete cessation of tachycardia. We then started isoproternol up to 10mcg/min with no induction of atrial tachycardia or atrial fibrillation. The patient was then observed overnight and discharged on 25mg of long acting metoprolol. He remains free from tachycardia three months post ablation. Repeat echocardiography demonstrated normalization of his LVEF.
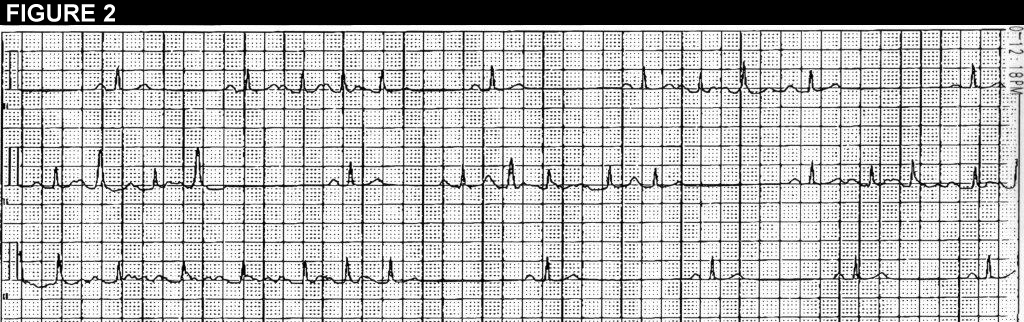
Despite an irregularly irregular rhythm, the patient in our case suffers from a focal atrial tachycardia. Focal atrial tachycardia as the sole mechanism for supraventricular tachycardia is relatively rare accounting for 10-15% of cases referred for catheter ablation.(1) The posterior wall of the left atrium is hypothesized to be a territory rich in triggers for the formation of atrial fibrillation.(2) Although relatively rare, sustained episodes of focal atrial tachycardia may lead to a rate related cardiomyopathy. Pulmonary vein associated tachycardia is a rare entity. In a retrospective series, only 3% of all atrial tachycardia from a large tertiary referral center was classified as pulmonary vein tachycardia.(3) In this series, focal ablation of either the earliest activation site at the os of the vein, or circumferential ablation of the culprit vein resulted in favorable long term freedom from recurrent atrial tachycardia, and atrial fibrillation. Pulmonary vein arrhythmias have been associated with the development of atrial fibrillation.(4) In three large series of patients undergoing ablation for focal pulmonary vein tachycardia, the reported development of atrial fibrillation post ablation is low.(5,6) While our patient has had improvement of his LVEF, and is free from arrhythmias, his future risk of the development of atrial fibrillation is unknown.
The best course for management of this patient, based on the history and figures 1 and 2, would be:
Show Answer