A 60-Year-Old Male Presents With Shortness of Breath and Leg Swelling
A 60-year-old male presented with progressive shortness of breath on exertion for the past six months with acute worsening in the past two to four weeks, accompanied with orthopnea and swelling of his legs. He denied any chest pain, pressure, palpitations or syncopal symptoms. He has been hospitalized twice in the past year for his shortness of breath and high blood pressure in different hospitals. He was prescribed 2l prn oxygen, for use with exertion six months ago at discharge during one of his hospitalizations.
Past Medical History
|
|
Medications
Amlodipine 10mg daily (started 4 weeks ago), Metoprolol 100mg twice daily, Clonidine 0.2mg tid, Hydrochlorothiazide 25mg daily, Lisinopril 40mg daily, Hydralazine 50mg tid, Metformin 500mg tid, Simvastatin 20mg daily, Aspirin 81mg daily
Physical Examination
- Heart Rate: 69bpm BP: 196/92mm Hg RR: 24/min Sat: 91% on 10l
- HEENT: JVP -5 cm at 45 degrees
- Cardiac: Regular rate and rhythm, normally split S1, S2, S4+, no murmur
- Lungs: bilateral crackles with vesicular breath sounds
- Abdomen: soft, non-tender with audible bowel sounds
- Peripherals: 2+ distal pulses bilaterally
- Extremities: 2+ pitting edema bilateral, around his ankles
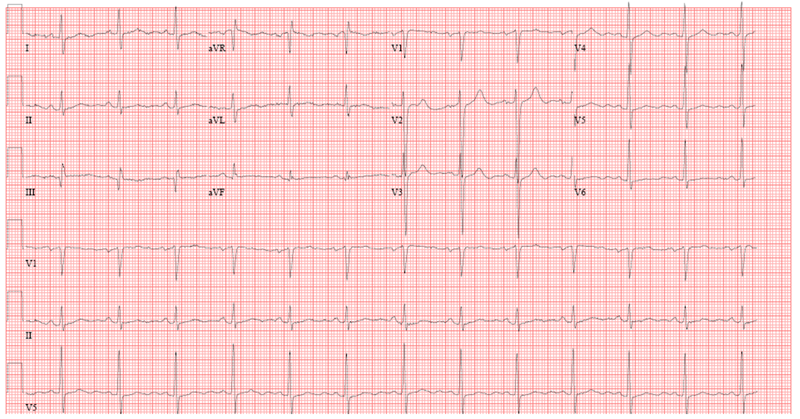
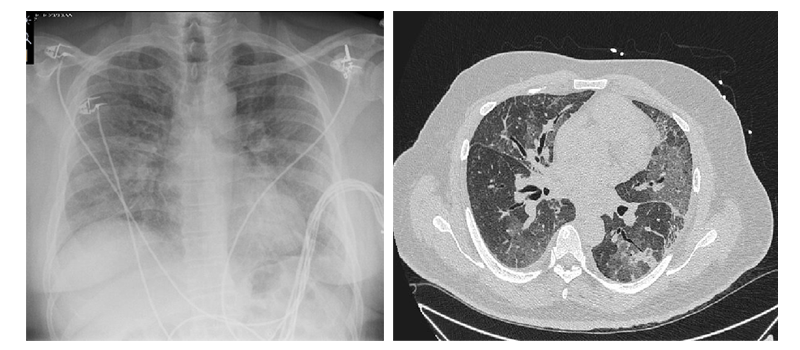
Data
- Hemoglogin 12.7gm/l
- White cell count 9.5
- LFTs normal
- BUN/Creatinine 29/1.4 mg/dl
- Troponin <0.01ng/ml
- NT pro BNP 90pg/ml
What is your diagnosis?
Show Answer