The Silent Bias: Risks of Not Following Clinical Guidelines in Developing Countries

There are several factors that are essential for personal development, but what are they? I am a firm believer that introspection is an important key to growth. After traveling to the U.S. from the island nation of the Dominican Republic to do a sub-internship, my interactions with residents, fellows and attendings have given me a new perspective on how medicine should ideally be practiced and has made me reflect on the issues that are silently affecting thousands of lives within my "Quisqueya La Bella" (Dominican Republic).
Clinical guidelines are ever-evolving to align with the latest evidence indicated by new research. In developing countries, most physicians do not have immediate access to these resources and often rely on old publications, along with the experience they have acquired during their careers, to care for their patients, which I think could represent a silent, and potentially harmful, bias in our local health system.

The COVID-19 pandemic has shown us how important it is to be up to date. It has become evident why new guidelines should be widely available. In my country, the Dominican Republic, the false information widely spread on social media about the "miraculous properties" of ivermectin and chloroquine, has led to a significant number of doctors prescribing these medications as prophylactic treatment, without having any data that support this notion. Due to this, the Ministry of Public Health had to publish a statement addressing the issue and clarified that these drugs have not been approved to treat COVID-19.
In fact, a similar issue is occurring in the field of cardiology. The results from my thesis (pending for open-access publication in the institutional repository RI-UNIBE) found that 27% of our sample from a local hospital did not follow the 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. This led to a second cardiovascular event in 13% of patients 14 days after their admission. We believe that this could have been reduced if a simple risk analysis, with the TIMI score, had been done before proceeding to a definitive strategy of management.
To elevate the quality of medical attention in developing countries, instead of focusing on the resources that we do not have, we must advocate for the adherence to clinical guidelines that are based on the best evidence available at the moment. Our medical decisions have an impact on someone's life, so staying up to date is of the utmost importance in providing the best care for our patients. I believe this could be achieved by raising awareness about the risks involved in making decisions based solely on experience. Equally important is the need to translate clinical guidelines into multiple languages to combat language barriers, improve the use of evidence-based treatment on a global scale, and ultimately provide clinicians the resources they need to treat their patients as they would like their loved ones to be treated.
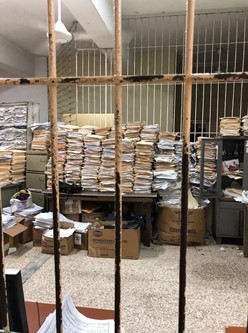
Acknowledgements: Special thanks to Vivian Valladares, MD, and Najib Shalabi, MD, for providing the pictures from inside a hospital in the Dominican Republic. Special thanks to Avery Carter, MD, for reviewing the article and all the support given during the rotation.

