Ten Points to Remember From the Recent Scientific Statement on Aortopathy Management in Children
Quick Takes
- Early genetic testing. Early genetic testing in children with aortopathy enables personalized care and early appropriate intervention, improving outcomes.
- Customized imaging. Tailored imaging modality, extent, and frequency are based on the genetic diagnosis, degree of aortic dilation, and growth rate.
- Multidisciplinary care. A multidisciplinary team approach ensures comprehensive management of both cardiovascular (CV) and non-CV aspects of pediatric aortopathy.
The scientific statement titled "Cardiovascular Management of Aortopathy in Children" from the American Heart Association (AHA) provides a comprehensive overview of aortopathy in pediatric patients and a consensus statement regarding management.1 Aortopathy includes various conditions that lead to the dilation, aneurysm, dissection, or rupture of the aorta and other blood vessels. It is commonly diagnosed in children and primarily affects the thoracic aorta, with potential involvement of peripheral vasculature. The pathogenesis of pediatric aortopathy often involves genetic conditions including connective tissue disorders and smooth muscle contraction disorders, as well as congenital heart conditions such as bicuspid aortic valve disease.
This scientific statement emphasizes the complexity of managing aortopathy in children, noting that management differs significantly from adults because of growth, developmental changes, and different risk profiles. Key components of management include genetic testing, cardiovascular (CV) imaging, medical therapy, lifestyle modifications, and surgical interventions tailored to the unique needs of pediatric patients. The statement aims to provide a general framework for the CV management of aortopathy in children, allowing for modifications based on individual characteristics of the child and their family, and to reduce variation in pediatric practice by combining available evidence and expert consensus.
Here are 10 key points to remember from this scientific statement:
- Aortopathy definition. Aortopathy encompasses conditions leading to aortic dilation, aneurysm, dissection, or rupture, and includes as examples Marfan syndrome, Loeys-Dietz syndrome, and vascular Ehlers-Danlos syndrome. Genetically mediated aortopathies affecting the thoracic aorta are often referred to as heritable thoracic aortic disease.
- Genetic testing. Early genetic testing is crucial for accurate diagnosis, risk stratification, and personalized management. (See Figure 2 in the AHA statement.1)
- Familial screening. Screening of first-degree relatives is advised, especially in families with a history of aortic disease, even when genetic testing has negative findings.
- Imaging modalities. Transthoracic echocardiography is the primary imaging modality, with cross-sectional imaging (magnetic resonance imaging/computed tomography angiography) recommended for detailed aortic assessment and in cases of suspected extravascular involvement. (Table 1; see Supplemental Tables 4, 6, and 7 in the AHA statement.1)
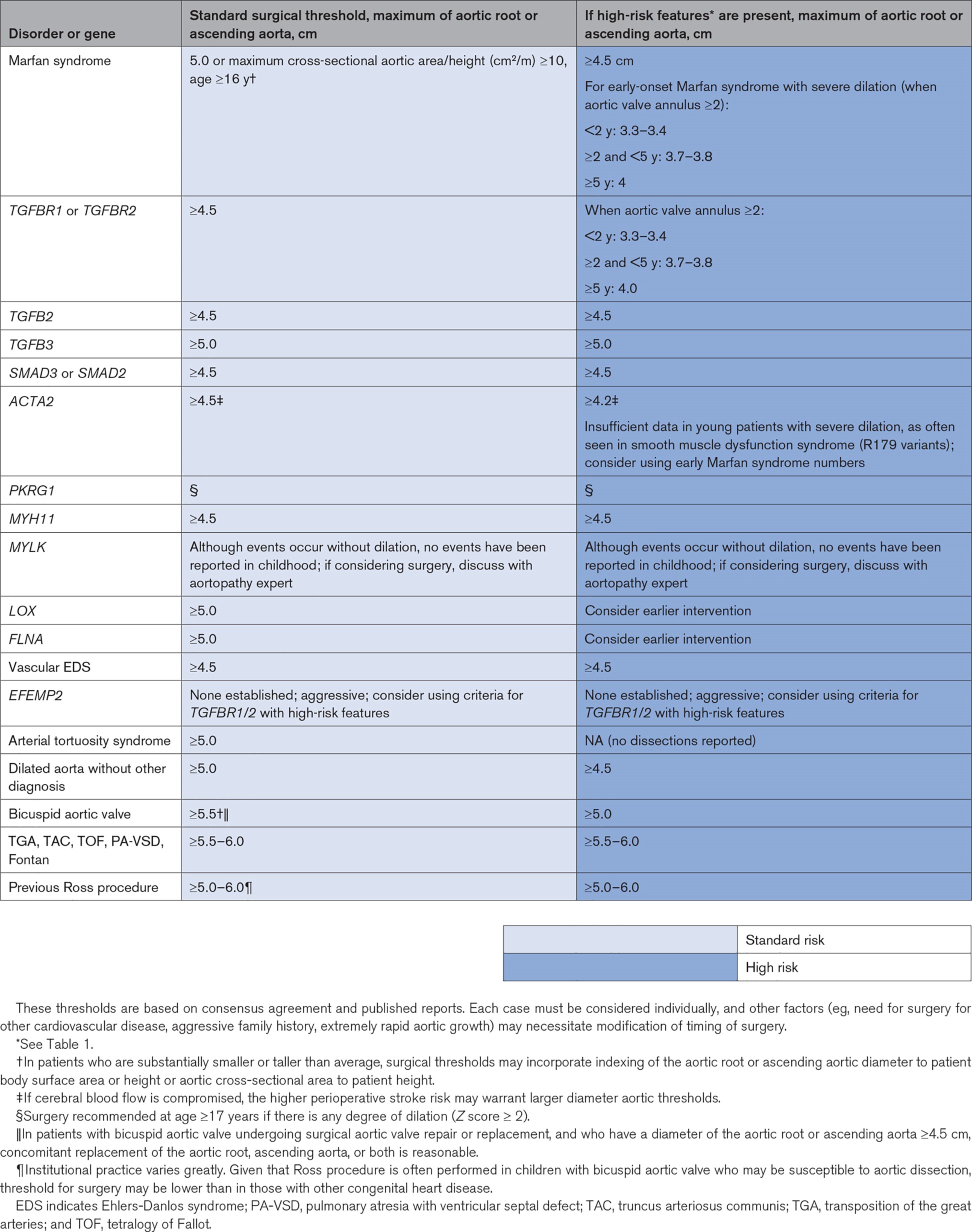
- Surveillance. Regular monitoring of aortic size using z scores, with frequency adjusted on the basis of aortic dilation severity and underlying genetic condition, is essential for managing progression. (Table 2)
- Medical therapy. Beta-blockers and angiotensin-receptor blockers are commonly used to slow aortic dilation, with therapy tailored to the individual's risk profile and genetic diagnosis. (See Table 3 in the AHA statement.1)
- Surgical intervention. Prophylactic aortic surgery is recommended on the basis of absolute aortic dimensions and the presence of high-risk features. Surgical thresholds vary depending on the underlying condition. (Table 2)
- Exercise guidance. Safe exercise practices should be encouraged, with limitations placed on activities that involve intense exertion or risk of trauma, especially in children with severe aortic dilation or connective tissue disorders. (See Table 4 in the AHA statement.1)
- Multidisciplinary care. Comprehensive management often requires a multidisciplinary team, including specialists in genetics, cardiology, and surgery, to optimize outcomes.
- Long-term management. Smooth transition to adult aortopathy care is vital, with a focus on ongoing surveillance and management to prevent complications such as dissection and rupture.
Table 1: Imaging Frequency Guidelines for Pediatric Aortopathy
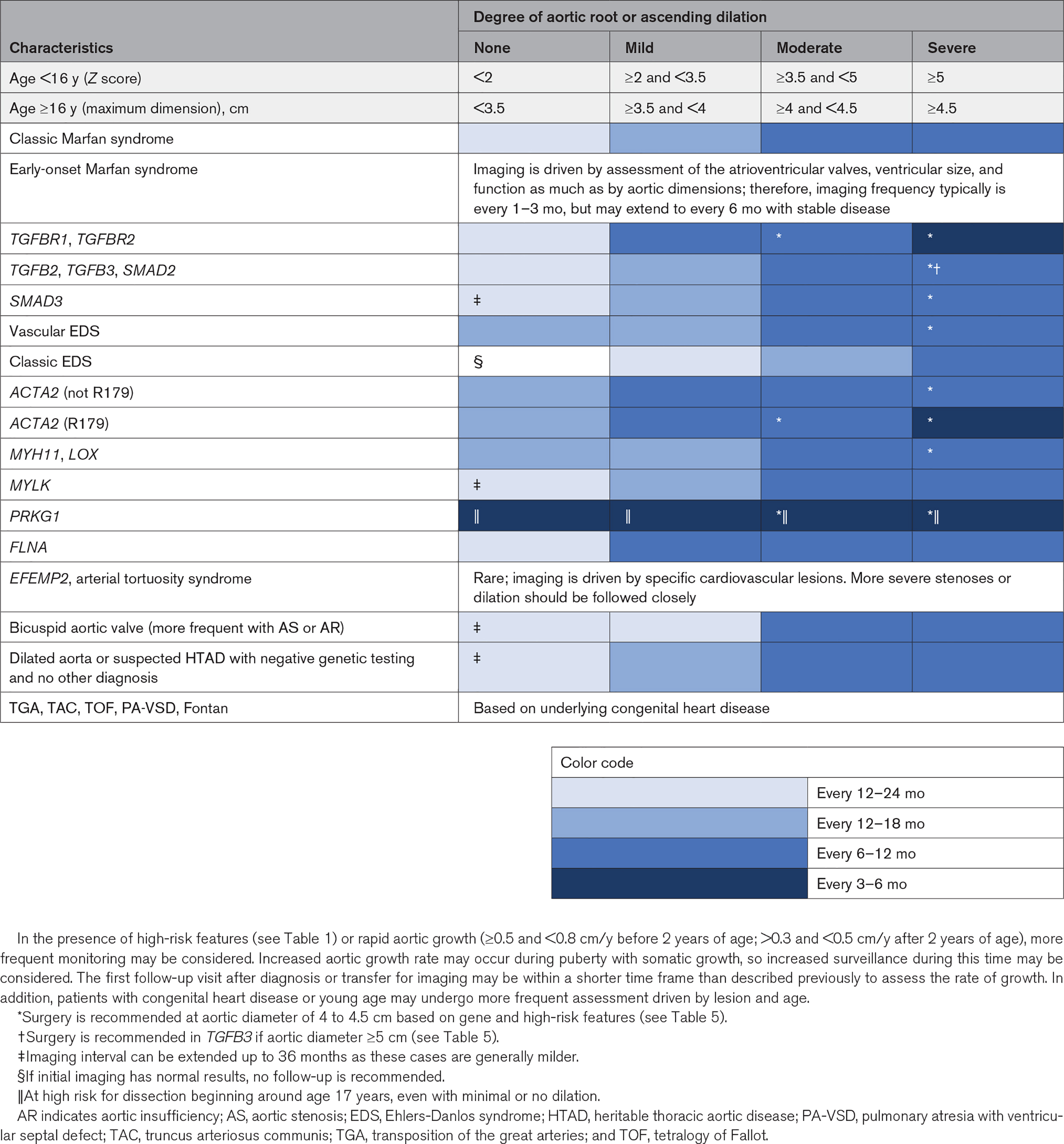
Table 2: Criteria for Aortic Root/Ascending Aortic Replacement
These points provide a framework for the CV management of pediatric aortopathy, emphasizing the importance of early diagnosis, regular monitoring, and individualized care. There is a need for more research to better understand the natural history and optimal management strategies for pediatric aortopathy. Future studies should focus on refining diagnostic criteria, improving imaging techniques, and developing targeted therapies.
References
- Morris SA, Flyer JN, Yetman AT, et al.; American Heart Association Council on Lifelong Congenital Heart Disease and Heart Health in the Young (Young Hearts), Council on Cardiovascular and Stroke Nursing; Council on Peripheral Vascular Disease, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Surgery and Anesthesia. Cardiovascular management of aortopathy in children: a scientific statement from the American Heart Association. Circulation 2024;150:e228-e254.
Clinical Topics: Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Vascular Medicine, Aortic Surgery, Cardiac Surgery and CHD and Pediatrics, Congenital Heart Disease
Keywords: Heart Defects, Congenital, Marfan Syndrome, Loeys-Dietz Syndrome, Aortic Valve, Aortic Aneurysm
