Why Is Cuff Size So Important and Other Factors That Affect Accurate Blood Pressure Measurement
Quick Takes
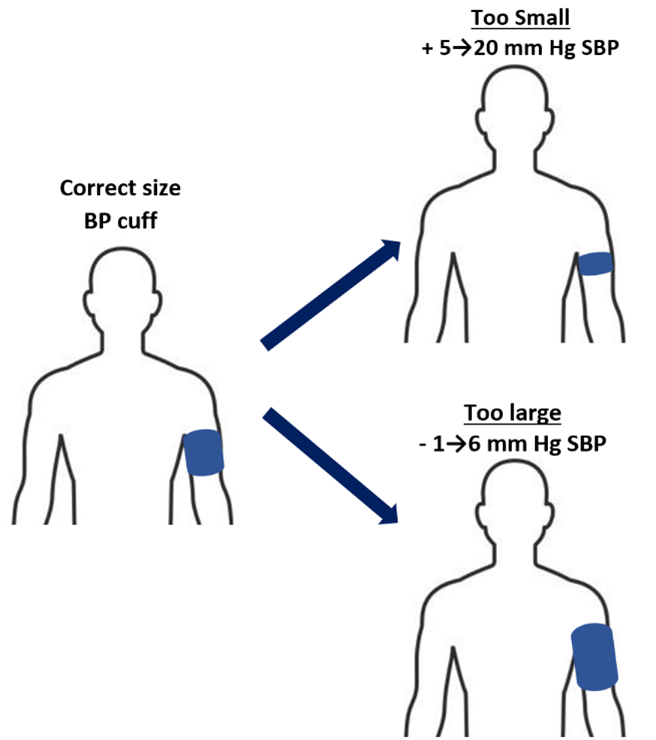
- Using a blood pressure (BP) cuff that is too small can result in up to a 20 mm Hg overestimation of systolic BP.
- Caffeine, alcohol, and over-the-counter medications can increase BP.
- Proper training and education of patients and clinicians are essential to ensure accurate BP measurement.
Hypertension is the most common cardiovascular disease (CVD) risk factor, with approximately 122 million persons in the United States meeting the diagnostic criteria and with it affecting >80% of adults ≥75 years of age.1,2 The accurate measurement of blood pressure (BP) is essential for the diagnosis, treatment, and control of hypertension, yet correct measurement technique is not regularly followed in clinical practice.3,4 Among persons with hypertension, higher BP levels also have implications for the timing and number of medications to be started.2 However, without accurate measurement of BP, clinicians cannot ensure patients are meeting their BP treatment goals.
Obtaining accurate BP measurements relies on patient and provider adherence to the recommended standardized protocols (Table 1). Given the increased emphasis on home BP readings, these techniques should be explained to patients so they may follow them when checking their BP outside of the office. However, behavior preceding BP assessment can also impact the reading, even if proper technique is followed.
Table 1: Best Practices and Common Pitfalls That Can Impact Accurate BP Measurement. Courtesy of Whelton S, Ebinger J, Yang E.
| Best Practices for BP Measurement | Common Measurement Pitfalls | Impact of Improper Practice on SBP (mm Hg) |
| Use appropriate cuff size | Cuff too small | + 5-20 |
| Cuff too large | - 1-6 | |
| Rest for 5 min before measurement | No rest period | + 10-20 |
| Sit quietly | Talking or texting during measurement | + 10-15 |
| Avoid caffeine for 30 min before measurement | Drinking coffee before measurement | + 5-8 |
| Have an empty bladder | Full bladder | +10-15 |
| Avoid alcohol consumption | Excess alcohol consumption | + 5-8 |
| Sit with back supported | Sitting upright on examination table | + 5-15 |
| Keep both feet flat on floor | Crossing legs, legs dangling from examination table | + 5-8 |
| BP cuff should be placed on bare arm | Measurement over clothing | ± 10-50 |
One such aspect of BP measurement is choosing the appropriately sized BP cuff (Figure 1). Often in a busy clinical practice or in environments where there are limited resources, a regular-sized BP cuff may be used for all patients.5 However, in a trial of 165 middle-aged adults, systolic blood pressure (SBP) measured using a regular-sized cuff in place of a small cuff resulted in a 3.8 mm Hg lower SBP reading, whereas use of a regular-sized cuff in place of a larger or extra-large cuff resulted in 4.8 and 19.7 mm Hg higher SBP readings, respectively.6 With use of an incorrect cuff size, 39% of participants were classified as having hypertension and 22% of participants with hypertension were classified as having normotension.
Figure 1: Difference in SBP With Use of Incorrect BP Cuff Size. Courtesy of Whelton S, Ebinger J, Yang E.
These results indicate that inaccurate BP measurement technique impacts not only the documented value but may also have a significant impact on hypertension classification, with implications for clinical care. The findings using a regular-sized cuff in place of an extra-large cuff were especially significant and are of particular importance given the increasing prevalence of overweight status and obesity that now affects >40% of US adults.1 Compounding this problem, hypertension is highly prevalent among individuals with overweight or obesity, high-risk groups for which proper BP control is especially effective, reducing the risk of CVD up to 25%.7
Additionally, clothing can impact the accuracy of BP measurement. Although a meta-analysis of 13 studies by David et al. reported no significant mean difference (+0.6 mm Hg SBP [p = 0.1]) in the measurement of BP over a thin sleeve, there may be greater variability in reported SBP differences at the individual patient level that may potentially cause misclassification between normotension and hypertension.8,9
There are other important considerations that can cause short-term changes in BP. Caffeine consumption can increase BP and avoiding caffeine for ≥30 min before BP measurement is therefore recommended. In a meta-analysis of five trials, it was found that consumption of 200-300 mg of caffeine raised SBP readings by 8.1 mm Hg.10 However, among persons who regularly consumed three to five cups of coffee per day for ≥2 weeks, there was no significant increase in mean 24-hour ambulatory BP. Conversely, although acute caffeine intake may raise BP, a reduction in the risk of CVD has been observed among persons who regularly consume a low to moderate amount of coffee.11 Therefore, caffeine consumption may be most important in the measurement of BP among occasional coffee drinkers and less so for regular coffee drinkers.
Patients may forgo emptying their bladder until after their clinical visit. However, a full bladder can increase the sympathetic tone, leading to higher BP measurements, and overactive bladder has been linked to a lower odds of BP control.12 For example, in one study among persons with a full bladder and the urge to urinate, SBP increased by 15 mm Hg and, after micturition, SBP returned to the normal range.13
Alcohol consumption in moderation (two or fewer drinks per day for men and one or no drinks per day for women) has been associated with decreased CVD risk in some studies.14 However, higher alcohol consumption is associated with increased BP and risk of hypertension. In a study of 9,681 participants whose weekly alcohol consumption was >300-499 mL, these participants had a 2.7 mm Hg higher SBP than nondrinkers and those who consumed ≥500 mL of alcohol had a 4.6 mm Hg higher SBP than nondrinkers.15 Excess or binge drinking was also associated with a large increase in SBP of 4.5 mm Hg. However, a reduction in alcohol intake has been associated with a stepwise decrease in BP.16
Over-the-counter medications may also impact BP. Among the most common are nonsteroidal anti-inflammatory drugs (NSAIDS), which increase BP through sodium retention. In the PRECISION-ABPM (Prospective Randomized Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen Ambulatory Blood Pressure Measurement) trial, patients randomized to ibuprofen had a 3.7 mm Hg increase in SBP (95% confidence interval, 1.7-5.6), which was 3.9 mm Hg higher than those randomized to celecoxib (p < 0.001).17 However, acetaminophen, which is often recommended as an alternative to NSAIDS, can also lead to higher BP measurements. In a recent double-blinded crossover trial, participants were randomized to either acetaminophen 4000 mg or placebo for 2 weeks. The mean SBP increased by 4.7 mm Hg (p < 0.001) in participants randomized to acetaminophen 4000 mg daily.18
Measuring BP accurately requires an understanding of the proper technique and the many different factors that can cause short-term and more persistent changes in BP. Choosing the correct BP cuff size is an especially important aspect among patients with overweight or obesity, who make up a growing percentage of the US adult population. Proper training and education for both clinicians and patients will help ensure that BP measurements more accurately reflect a patient's true resting BP. In addition, a knowledge of factors that have a short-term effect on BP can help reduce the risk of measurement error and allow for better interpretation of readings that may change from one measurement to the next.
References
- Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation 2022;145:e153-e639.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APha/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127-e248.
- Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019;73:e35-e66.
- Elias MF, Goodell AL. Human errors in automated office blood pressure measurement: still room for improvement. Hypertension 2021;77:6-15.
- Taler SJ, Brady TM. The challenge of accurate blood pressure measurement: optimizing cuff size and fit is important for all, not just for some. Am J Hypertens 2022;35:503-5.
- Brady TM, Charleston J, Ishigami J, et al. Abstract EP01: One size does not fit all: impact of using a regular cuff for all blood pressure measurements. Circulation 2022;145:AEP01. Available at: https://www.ahajournals.org/doi/10.1161/circ.145.suppl_1.EP01. Accessed 06/02/2023.
- Wright JT Jr, Williamson JD, Whelton PK, et al.; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103-16.
- Ishak A, Juraschek SP, Cluett J. Clothing and blood pressure measurement precision. J Hypertens 2021;39:381-2.
- Seguret D, Gamelon D, Dourmap C, Steichen O. Blood pressure measurements on a bare arm, over a sleeve or below a rolled-up sleeve: a systematic review and meta-analysis. J Hypertens 2020;38:1650-8.
- Mesas AE, Leon-Muñoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr 2011;94:1113-26.
- Ding M, Bhupathiraju SN, Satija A, van Dam RM, Hu FB. Long-term coffee consumption and risk of cardiovascular disease: a systematic review and a dose-response meta-analysis of prospective cohort studies. Circulation 2014;129:643-59.
- Akbar A, Liu K, Michos ED, et al. Association of overactive bladder with hypertension and blood pressure control: the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens 2022;35:22-30.
- Fagius J, Karhuvaara S. Sympathetic activity and blood pressure increases with bladder distension in humans. Hypertension 1989;14:511-7.
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671.
- Marmot MG, Elliott P, Shipley MJ, et al. Alcohol and blood pressure: the INTERSALT study. BMJ 1994;308:1263-7.
- Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension 2001;38:1112-7.
- Ruschitzka F, Borer JS, Krum H, et al. Differential blood pressure effects of ibuprofen, naproxen, and celecoxib in patients with arthritis: the PRECISION-ABPM (Prospective Randomized Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen Ambulatory Blood Pressure Measurement) trial. Eur Heart J 2017;38:3282-92.
- MacIntyre IM, Turtle EJ, Farrah TE, Graham C, Dear JW, Webb DJ; PATH-BP (Paracetamol in Hypertension–Blood Pressure) Investigators. Regular acetaminophen use and blood pressure in people with hypertension: the PATH-BP trial. Circulation 2022;145:416-23.
Clinical Topics: Prevention, Statins, Hypertension, Pulmonary Hypertension and Venous Thromboembolism
Keywords: Primary Prevention, Secondary Prevention, Cardiovascular Diseases, Hypertension, Overweight, Obesity, Risk Factors, Blood Pressure Monitoring, Ambulatory, Anti-Inflammatory Agents, Non-Steroidal, Reference Values, Caffeine, Urination, Celecoxib, Ibuprofen, Acetaminophen, Naproxen, Cross-Over Studies, Confidence Intervals, Prospective Studies, Goals
< Back to Listings