New ACC, AHA, HFSA Guideline Updates Recommendations For Managing HF
"Patient-centric recommendations" to help clinicians prevent, diagnose and treat heart failure (HF) are the focus of a new clinical guideline released April 1 by the ACC, the American Heart Association, and the Heart Failure Society of America and simultaneously published in the Journal of the American College of Cardiology.
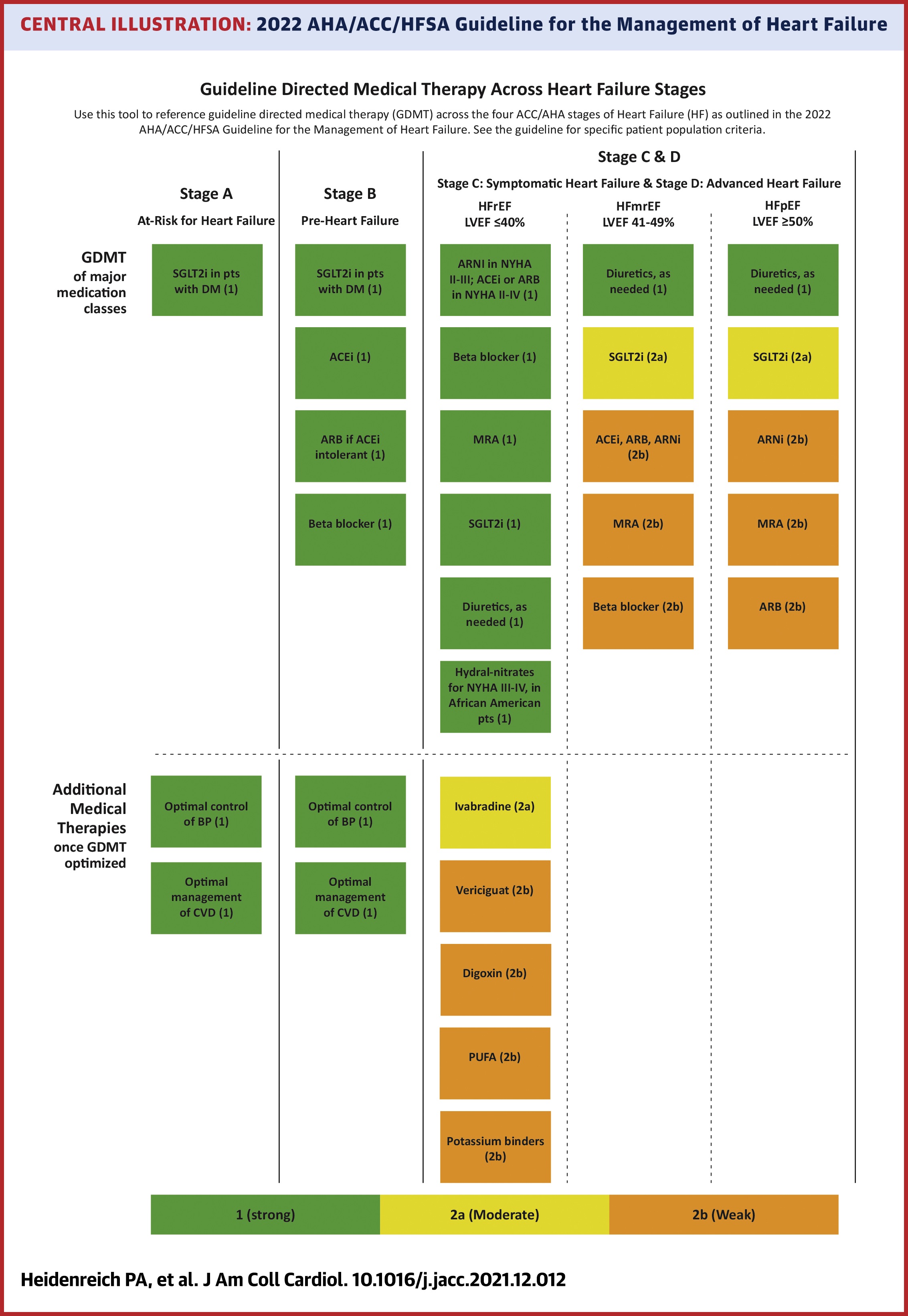
The joint 2022 Guideline for the Management of HF includes a focus on HF prevention, with revised definitions of Stage A and Stage B HF intended to identify risk factors early (Stage A) and provide treatment before structural changes or signs of decreased HF occur (Stage B).
"One primary goal with the new guideline was to use recently published data to update our recommendations for the evaluation and management of heart failure," said Paul A. Heidenreich, MD, MS, FACC, guideline writing committee chair. "One focus was prevention of heart failure through optimizing blood pressure control and adherence to a healthy lifestyle."
While Stage A recommendations for at-risk patients are also applicable for those individuals who have progressed to Stage B and have "pre-HF" symptoms, additional medications to prevent symptomatic HF are recommended. Specifically, ACE-inhibitors (ACEi) are suggested for patients with left ventricular ejection fraction (LVEF) ≤40%, while angiotensin receptor blockers (ARBs) may be prescribed for individuals with an intolerance or contraindication to ACEi. Cholesterol-lowering statins are recommended for people with a history of a myocardial infarction or acute coronary syndrome.
The use of multidisciplinary teams to facilitate guideline-directed medical therapy and self-care support for learning to manage symptoms are recommended in managing individuals who have progressed to Stage C and have HF symptoms. Screenings to identify potential medical or social barriers for effective self-care are also encouraged, as well as education and support to reduce rehospitalization and improve survival. Individuals with Stage C should also be fully vaccinated against respiratory illnesses including COVID-19.
For individuals with Stage C, the new guideline also refines the current four classifications of HF based on LVEF with new terminology:
- HF with reduced ejection fraction (HFrEF) includes people with LVEF ≤40%.
- HF with improved ejection fraction (HFimpEF) includes individuals with previous LVEF ≤40% and a follow-up measurement of LVEF >40%.
- HF with mildly reduced ejection fraction (HFmrEF) includes people with LVEF 41-49% and evidence of increased LV filling pressures.
- HF with preserved ejection fraction (HFpEF) includes individuals with LVEF ≥50% and evidence of increased LV filling pressures.
Pharmacological treatment for managing patients across the four classifications of HF are also addressed by the guideline. Recommended treatment for those with HFrEF includes four classes of medications, in addition to diuretics. Use of angiotensin receptor-neprilysin inhibitors (ARNis) is recommended, and if not feasible, the use of ACEi is recommended. ARBs are recommended for individuals with an intolerance or potential adverse reaction to ACEi medicines. Mineralocorticoid receptor antagonists (MRA) or beta-blockers are also recommended as in the prior guideline. SGLT2 inhibitors (SGLT2i) are now recommended for people with symptomatic chronic HFrEF regardless of the presence or absence of type 2 diabetes.
"After careful evaluation of new evidence, guideline-directed medical therapy now includes four medication classes that include SGLT2 inhibitors. Irrespective of diabetes status, the DAPA-HF and EMPEROR trials have shown the benefit of treating patients with HFrEF with SGLT2 inhibitors, showing a 30% reduction in heart failure rehospitalization. This is a major step forward in reducing mortality rates in this vulnerable population," said Biykem Bozkurt, MD, PhD, FACC, guideline writing committee vice-chair.
Individuals with HFmrEF should be treated first with an SGLT2i along with diuretics as needed, according to the guideline authors. ARNi, ACEi, ARB, MRA and beta-blockers are considered weaker recommendations in this population, as the evidence in this population is less robust. As LVEF may change over time, people with HFmrEF should have repeat evaluations of LVEF.
People with HFpEF and hypertension should aim for blood pressure targets in accordance with clinical guidelines. For people with HFpEF, the guideline suggests that SGLT2i may be beneficial in decreasing HF hospitalizations and cardiovascular mortality. Management of atrial fibrillation can also improve symptoms. In select individuals with HFpEF, MRAs, ARBs and ARNi may be considered, particularly among people with LVEF on the lower end of the spectrum of HFpEF.
The guideline also includes recommendations for ICDs, CRT and diagnosis and treatment of cardiac amyloidosis. For those with amyloid heart disease, new recommendations for treatment including screening for serum and urine monoclonal light chains, bone scintigraphy, genetic sequencing, tetramer stabilizer therapy and anticoagulation.
Specialty referrals for individuals with Stage D advanced HF, recommendations for management of atrial fibrillation and valvular heart disease in patients with HF are also included in the guideline. As are recommendations for select patients with anemia, hypertension, sleep disorders and type 2 diabetes. Other topics, including pregnancy and cardio-oncology are also a focus. In keeping with other recent guidelines, value statements were created for select recommendations where high-quality, cost-effectiveness studies of the intervention have been published.
This new guideline replaces the 2013 ACCF/AHA Guideline for the Management of Heart Failure and the 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure.
Don't miss these ACC.22 sessions: Party Like It's 2022: The Latest Guidance in Heart Failure Care, on Saturday, April 2 at 4:15 p.m.; Clinical Spotlight Series SGLT2is: The New Pillar in Heart Failure Care, on Sunday, April 3 at 5:30 p.m., and Heart Failure Highlights, on Monday, April 4 at 2:30 p.m. Learn more and register for ACC.22 here.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Valvular Heart Disease, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and VHD, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Heart Transplant, Mechanical Circulatory Support, Interventions and Imaging, Interventions and Structural Heart Disease, Echocardiography/Ultrasound, Exercise, Hypertension, Sleep Apnea
Keywords: Amyloidosis, Anemia, Atrial Fibrillation, Biomarkers, Cardiac Catheterization, Cardiac Resynchronization Therapy, Defibrillators, Implantable, Pacemaker, Artificial, Cardiology, Cardiac Rehabilitation, Rehabilitation, Cardiomyopathies, Delivery of Health Care, Delivery of Health Care, Integrated, Organization and Administration, Comorbidity, Heart Failure, Diagnostic Techniques, Cardiovascular, Diabetes Mellitus, Drug Therapy, Echocardiography, Biopsy, Myocardium, Exercise, Exercise Test, Functional Residual Capacity, Genetic Diseases, Inborn, Guideline, Practice Guideline, Therapeutics, Heart Transplantation, Hemodynamics, Hypertension, Diagnostic Imaging, Heart-Assist Devices, Sleep Apnea, Obstructive, Palliative Care, Patient-Centered Care, Motor Activity, Pregnancy, Primary Prevention, Secondary Prevention, Myocardial Revascularization, Risk Factors, Risk Assessment, Self Care, Shock, Sleep Apnea Syndromes, Patient Care Team, Transitional Care, Heart Valve Diseases
< Back to Listings