This 56-year-old woman with systemic AL amyloid and biopsy-proven cardiac involvement developed recurrent atrial arrhythmias during the course of her chemotherapy and autologous stem-cell transplant. Anticoagulation and amiodarone were commenced and external cardioversion was performed for restoration of sinus rhythm, but arrhythmia recurrence with rapid ventricular rates ensued. She was referred for further evaluation because of marked exercise intolerance.
Baseline 12-lead ECG is shown in figure 1. On echocardiography, her left atrial dimension was 4.0 cm in diameter and LV ejection fraction was 50% with Doppler trans-mitral flow evidence for diastolic function.
The correct answer is: D. Electrophysiological study and possible catheter ablation for atrial arrhythmias
The baseline 12-lead ECG shows discrete P waves evident in several leads, such as V1, aVL, and III. However, close inspection reveals irregular intervals and varying morphology. After discussing various alternatives, the patient elected to have an attempt at catheter ablation.
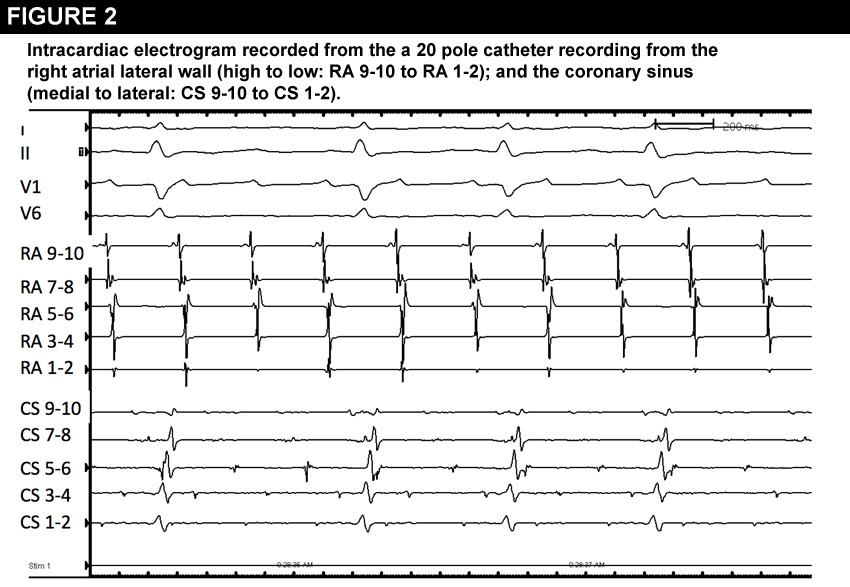
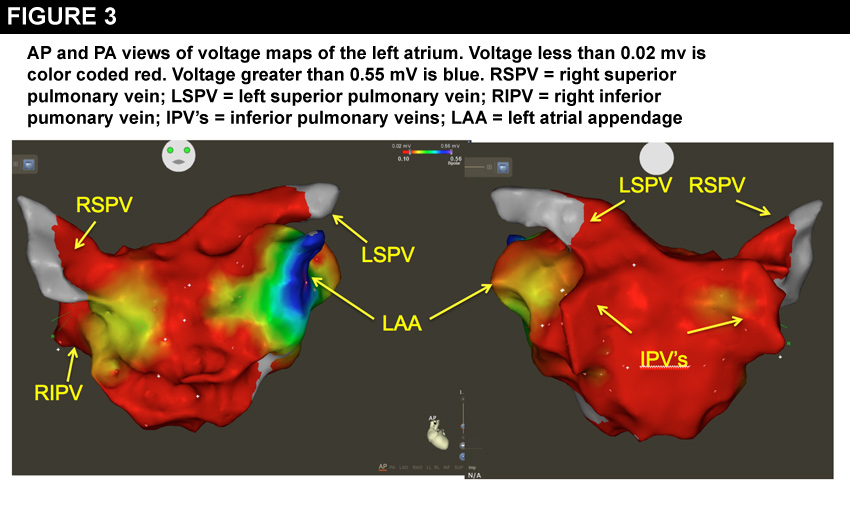
At electrophysiological study, right atrial activation was consistently cephalo- caudal in the lateral right atrium with tachycardia cycle length ranging between 250 to 270 msec. Fractionated, irregular low amplitude electrograms were present in the coronary sinus suggesting fibrillatory wavefronts (figure 2). There was spontaneous oscillation in tachycardia cycle length (figure 2). Left atrial electrogram voltage mapping was performed using a 3-D electroanatomic mapping system (Carto Mapping system, Johnson and Johnson Ltd, Cincinatti, OH) (figure 3). Voltage mapping revealed marked diminution of electrical voltages to below 0.02 millivolts throughout the left atrium, except on the septum near the right superior pulmonary vein and left atrial appendage, where voltages exceeded 1.5 mV. Typically, normal endocardial left atrial bipolar voltages average 1.5 mV.
(1) Hence, the low voltages recorded in this case represent amyloid infiltration of the left atrium and/or fibrosis.
Radiofrequency (RF) ablation targeting areas of complex fractionated electrograms in the left atrium along the pulmonary vein antrum, and left atrial roof converted the rhythm to a slower, regular left atrial tachycardia that terminated with ablation in the left atrial septum inferior to the right superior pulmonary vein. Programmed stimulation was then performed and cavotricuspid isthmus dependent atrial flutter was induced. Ablation along the cavotricuspid isthmus to create conduction block in this isthmus terminated the arrhythmia to normal sinus rhythm. She remains arrhythmia-free during 18 months of follow up off amiodarone. Chronic anticoagulation has been continued due to absence of evidence for left atrial contraction by echocardiography.
Concerning treatment alternatives, it is highly unlikely that another anti-arrhythmic agent, such as sotalol or dofetilide would have greater efficacy in this patient and may have more potential for pro-arrhythmic polymorphic ventricular tachycardia. Cardiac transplantation is not a usual consideration because it is associated with a high incidence of recurrent amyloid deposition in the grafts and survival is limited by the effects of extra-cardiac amyloidosis.(2) AV node ablation and pacemaker implant is a reasonable alternative, but may necessitate a more complex biventricular pacing system and renders the patient pacemaker dependent. In addition, patients with severe diastolic heart failure, such as those with hypertrophic cardiomyopathy and infiltrative diseases, may fare better in sinus rhythm rather than a regular paced rhythm, despite impaired contraction of the left atrium.
Cardiac amyloidosis refers to infiltration of the myocardium with amyloid fibrils, usually as part of a systemic disease. Less frequently, localized infiltration of the myocardium is responsible, and may appear isolated to the atria.(3) Diastolic left ventricular dysfunction and right heart failure are the presenting feature in 50% of patients. Conduction system disease, syncope, postural hypotension and atrial arrhythmias are the other forms of presentation. Atrial involvement in cardiac amyloidosis has not been studied in detail.(4, 5) In most cases, atrial arrhythmia is usually classified as atrial fibrillation (AF). However, extensive disruption of conduction due to amyloid infiltration and/or fibrosis is common and results in a relatively organized appearance to AF. In the majority, multiple focal and re-entrant atrial tachycardias are common. In the present case, fibrillatory wave fronts quickly organized to atrial tachycardias with minimal left atrial substrate modification allowing for successful termination with further RF ablation specifically targeting re-entrant circuits.
References
- Lemery R, Birnie D, Tang ASL, et al. Normal atrial activation and voltage during sinus rhythm in the human heart: an endocardial epicardial mapping study in patients with a history of atrial fibrillation. J Cardiovasc Electrophysiol 2007; 18: 402-8.
- Selvanayagam JB, Hawkins PN, Paul B, et al. Evaluation and management of cardiac amyloidosis. J Am Coll Cardiol 2007; 50: 210 -10.
- Dubrey SW, Hawkins PN, Falk RH. Amyloid disease of the heart: assessment, diagnosis and referral. Heart 2011; 97: 75-84.
- Murtagh B, Hammill SC, gertz MA, et al. Electrocardiographic findings in primary systemic amyloidosis and biopsy-proven cardiac involvement. Am J Cardiol 2005; 95: 535-7.
- Falk RH, Rainbow A, Cohen AS. Cardiac arrhythmias in systemic amyloidosis; correlation with echocardiographic abnormalities. J Am Coll Cardiol 1984; 3: 107-13.