The best next step is cMRI. Whereas both stress echocardiography and provocative maneuvers assess dynamic LVOT obstruction, cMRI provides superior detail in evaluating cardiac structure, myocardial composition, and conditions such as hypertrophic cardiomyopathy (HCM).1 Given the abnormal T-wave changes seen on ECG and the hypertrophy seen on echocardiogram, cMRI offers a more comprehensive assessment, particularly for identifying fibrosis, apical hypertrophy, or other subtle features that may guide management.
Coronary angiography, exercise stress test, and Holter monitor are unnecessary without ischemic or arrhythmic concerns. TEE adds little value, and gradual return to activity would be premature without clearer structural evaluation, making cMRI the best next step.
ECG Findings
The abnormal T-wave changes seen in this patient's ECG, including elevated T-wave voltages, lateral TWI, anteroseptal J-point elevation, and inferior TWI, are concerning and require further evaluation (Image 1). Although these findings may suggest HCM, they are considered abnormal in athletes on the basis of international criteria, distinguishing them from training-induced hypertrophy. This highlights the need for additional diagnostic imaging to clarify the underlying etiology. Even if the initial workup has unremarkable findings, approximately 7% of athletes with these findings may go on to develop HCM, underlining the importance of serial follow-up.
Image 1

Echocardiogram Findings
The echocardiogram had findings of a normal-sized LV with mild septal and moderate posterior hypertrophy, along with apical cavity obliteration. The LVEF was 75%, and no LVOT obstruction was seen, ruling out hypertrophic obstructive cardiomyopathy. Although reassuring, these findings require further imaging to assess the etiology of the hypertrophy, as training-induced adaptations and pathological hypertrophy can appear similar.
cMRI Findings
The cMRI had remarkable findings (Image 2):
- LV. Normal size with wall thickness 1.1 cm (anteroseptal and inferolateral); LVEF 59%, which is within normal range for an athlete (52-69%). No myocardial scar on postgadolinium imaging. Prominent apical insertion of the papillary muscles, a benign variation common in athletes.
- Extracellular volume (ECV). Measured at 23.2% in the apex and 25% in the basal septum, both within normal limits, suggesting physiological hypertrophy without significant myocardial fibrosis or pathology such as HCM.
- Right ventricle (RV). Normal size and function, RV ejection fraction 54% (>45%).
- Valvular findings. No significant valvular disease.
Image 2
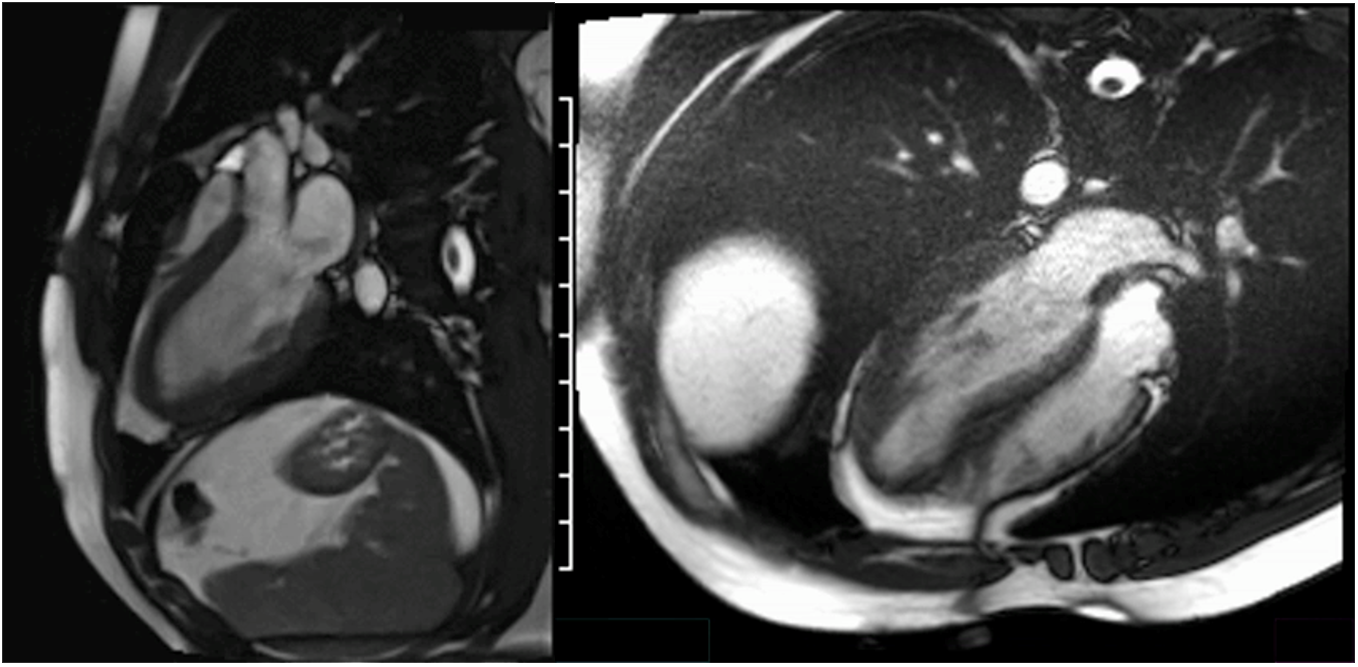
The inclusion of the ECV measurements is particularly important in distinguishing between normal myocardial tissue and pathological changes. The normal ECV values suggest no significant myocardial fibrosis or abnormal myocardial tissue composition, further supporting the suspicion that the hypertrophy observed on echocardiogram was likely due to athletic training rather than HCM.
Discrepancy Between Echocardiography and cMRI
The echocardiogram findings raised concerns about potential pathological hypertrophy, including apical cavity obliteration and hyperdynamic function, prompting further evaluation with cMRI. cMRI offers superior spatial resolution and myocardial tissue characterization, providing a clearer assessment that can clarify discrepancies observed on echocardiography.
Although the echocardiogram findings suggested apical cavity obliteration, this was not confirmed by cMRI. Discrepancies may have arisen from differences in image quality, particularly in visualizing the endocardium and myocardial structures. Additionally, hemodynamic changes such as dehydration (which is common in athletes) can sometimes contribute to apical cavity obliteration and should be considered alongside potential issues with image quality. For instance, echocardiographic wall thickness measurements can vary depending on image quality and the location of the papillary muscles and chordae. The cMRI more clearly visualized the prominent apical insertion of the papillary muscles, which were likely mistaken for the endocardium on echocardiography, creating the appearance of apical cavity obliteration and hyperdynamic function. The cMRI findings confirmed normal apical tapering and thickness, supporting the absence of pathological findings.
The cMRI findings, including normal wall thickness and no myocardial fibrosis, suggested that the hypertrophy was likely physiological rather than pathological. This differentiation is critical in athletes, as distinguishing between an athletic heart and HCM impacts both management and sports participation.
Guidelines for Sports Cardiologists
The 2024 multisociety Guideline for the Management of HCM highlights the role of cMRI in distinguishing between athletic heart and pathological conditions such as HCM, particularly when evaluating left ventricular hypertrophy (LVH) in athletes.1 This is essential for differentiating between normal, training-induced hypertrophy and pathological hypertrophy, which may indicate HCM.
A key challenge is the gray zone, in which LVH features overlap between physiological adaptations and pathological conditions. In this context, ECV measurement via cMRI is an important tool for assessing myocardial fibrosis.2 An elevated ECV may suggest pathological hypertrophy, such as HCM, whereas a normal ECV typically points to physiological hypertrophy in athletes. However, ECV should not be used in isolation.2 Additional parameters, such as LV mass index, ECG findings, and genetic testing findings, are advised to provide a comprehensive assessment.1 This integrated approach helps avoid misdiagnosis, ensuring athletes are neither unfairly restricted from sports nor exposed to risks such as sudden cardiac arrest and death associated with HCM.
By incorporating advanced imaging, sports cardiologists can make more informed, shared decisions with athlete patients, offering optimal care while distinguishing between normal adaptations and potentially dangerous conditions.
Alternative Approaches
Although a gradual return to activity with symptom monitoring would be reasonable, there was a lack of diagnostic clarity given the remarkable ECG and echocardiogram findings. A cMRI offers a definitive evaluation, ensuring there are no significant structural abnormalities that could jeopardize the athletes' health during intense activity and allowing health care providers to assess their safe participation in competitive sports.
References
- Writing Committee Members, Ommen SR, Ho CY, et al. 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol 2024 Oct 29;84:1771]. J Am Coll Cardiol 2024;83:2324-2405.
- Nelson K, LaRocca G. Left Ventricular Hypertrophy in Athletes: Elucidating the Gray Zone Through cMRI Tissue Characterization Beyond LGE. http://www.acc.org. Oct 15, 2024. Accessed 02/10/2025. https://www.acc.org/latest-in-cardiology/articles/2024/10/15/10/39/left-ventricular-hypertrophy-in-athletes.