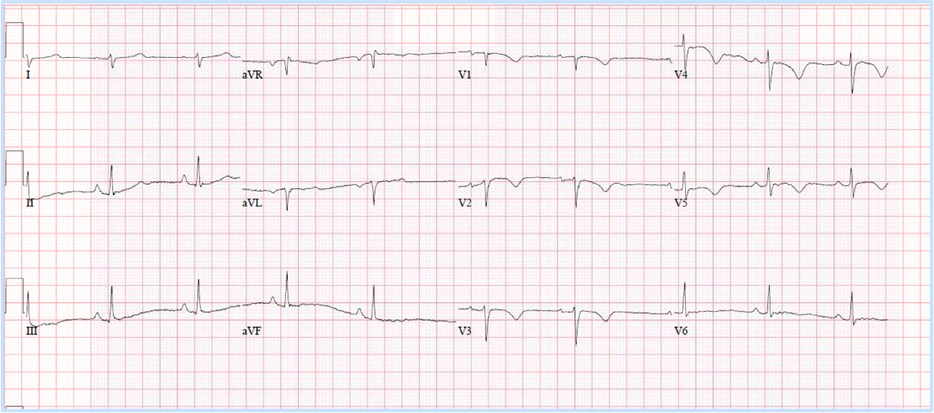
This patient's ECG had notable findings of TWI throughout the anterior precordial leads without improvement during exercise testing, which is concerning for an underlying cardiomyopathy. She required further diagnostic workup.
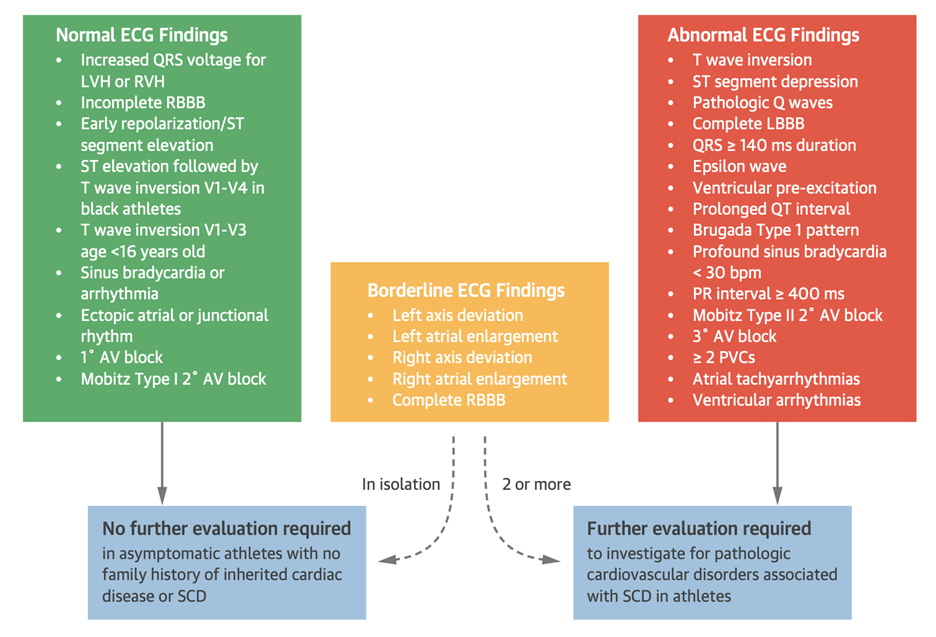
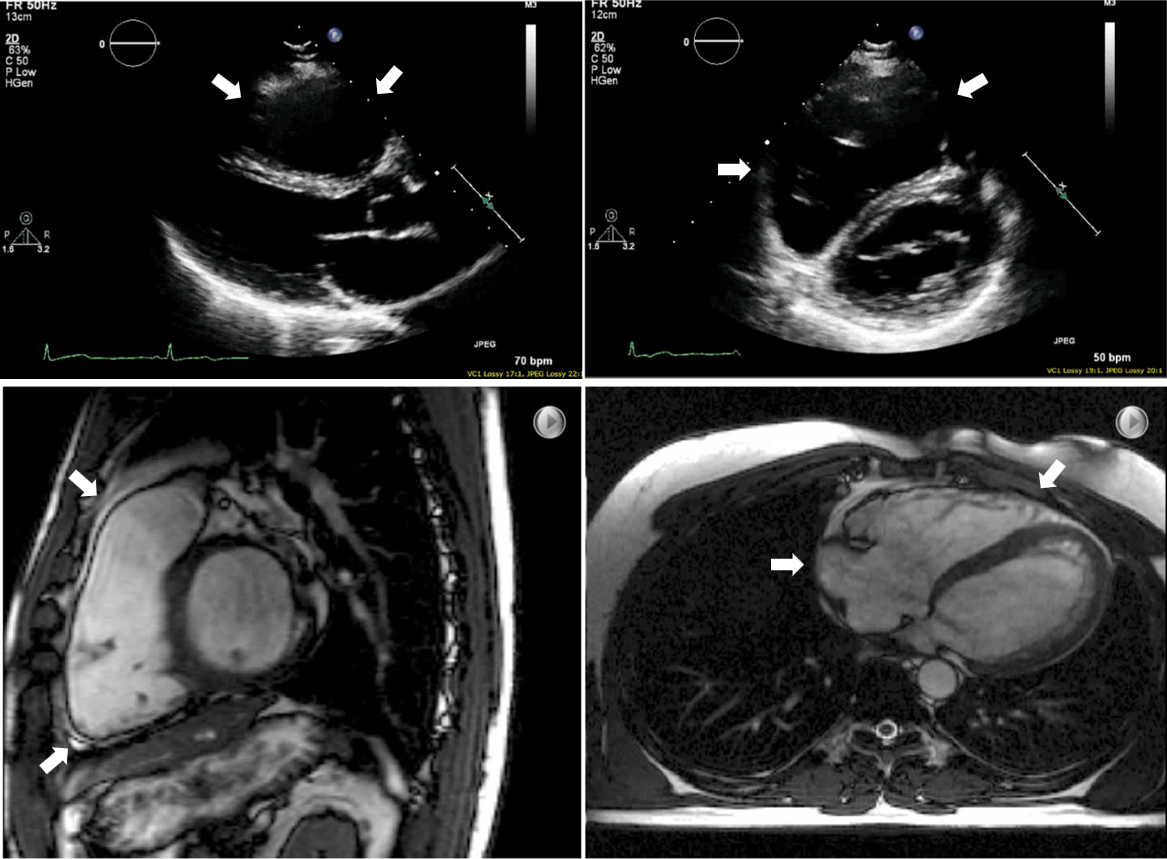
When TWI are detected on an athlete's ECG, the first priority should be to determine whether they represent a normal physiologic response to training or a potential underlying pathology. ECG findings representing normal physiologic adaptation to exercise are summarized in Figure 1, adapted from the current consensus statement on ECG interpretation in athletes—the International Criteria published in 2018.1 In particular, two distinct patterns of TWI are considered normal variants: the juvenile pattern of TWI seen in athletes <16 years of age and the early repolarization pattern of ST-segment elevation followed by TWI (previously referred to as the Black athlete pattern).
Figure 1: International Consensus Standards for ECG Interpretation in Athletes
Reprinted with permission from Sharma S, Drezner JA, Baggish A, et al. International recommendations for electrocardiographic interpretation in athletes. J Am Coll Cardiol 2017;69:1057-75.
1° = first-degree; 2° = second-degree; 3° = third-degree; AV = atrioventricular; ECG = electrocardiogram; LBBB = left bundle branch block; LVH = left ventricular hypertrophy; PVC = premature ventricular contraction; RBBB = right bundle branch block; RVH = right ventricular hypertrophy; SCD = sudden cardiac death.
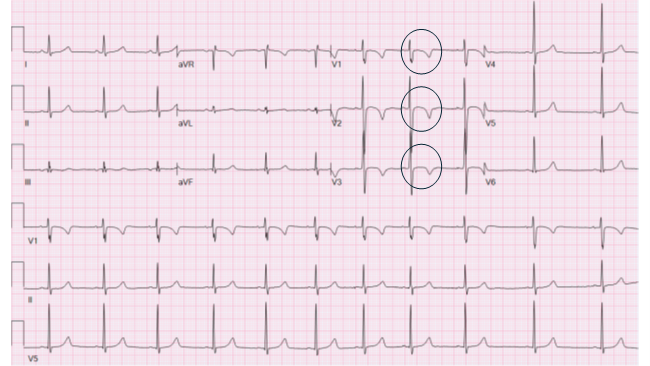
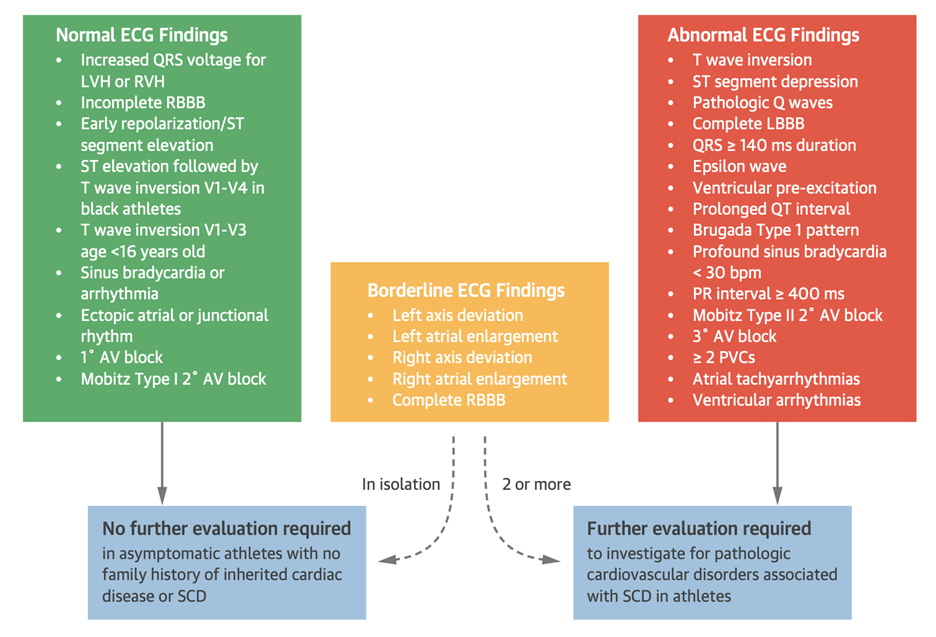
The juvenile ECG pattern (Figure 2) consists of TWI isolated to the anterior precordial leads (V1 through V3). One study identified this pattern in 16% of athletes <16 years of age, although the TWI normalized during 4 years of follow-up in 94% of the children.2 As such, it is considered a benign finding in athletes <16 years of age but not in older individuals. Given this patient's age, extension of TWI beyond leah V3, and lack of normalization with exercise, her baseline and stress ECG findings should not be considered consistent with the juvenile ECG pattern.
Figure 2: Juvenile ECG Pattern Characterized by TWI in Leads V1 Through V3 in an Athlete <16 Years of Age
The TWIs are circled.
ECG = electrocardiogram; TWI = T-wave inversions.
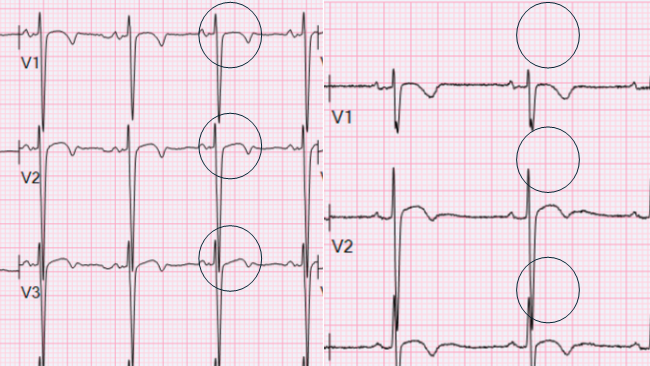
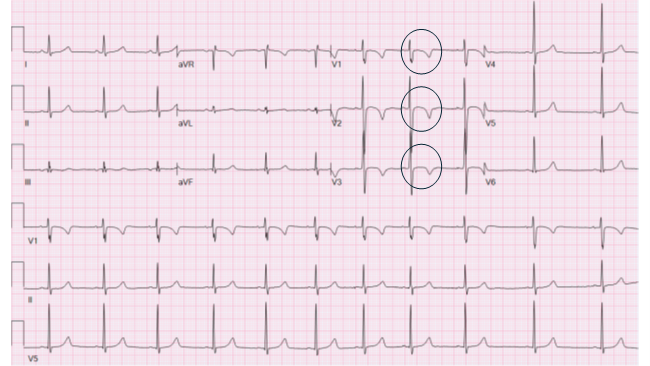
The early repolarization pattern is characterized by TWI in leads V1 through V4 associated with J-point elevation and convex ST-segment elevation (Figure 3).3 This constellation of findings occurs most commonly in athletes of Afro-Caribbean descent, although it is found in lower numbers in other ethnicities as well. Older literature, including the International Criteria, referred to this as the Black athlete pattern, although expert consensus now recommends against the use of race-based terminology and criteria in sports cardiology.4 As such, this pattern is now considered a benign repolarization variant in all athletes in the absence of other remarkable findings on ECG.5 Extension of TWI to the lateral leads, as seen in this athlete, may represent a normal variant in certain athletes but is the predominant distribution of TWI in hypertrophic cardiomyopathy (HCM).5 As such, lateral extension of TWI beyond lead V4 necessitates further investigation.
Figure 3: Early Repolarization Patterna Characterized by J-Point Elevation Followed by TWI in Leads V1 Through V3b
a Previously referred to as Black athlete pattern
b These can extend to lead V4 and rarely to the lateral leads
The TWIs are circled.
ECG = electrocardiogram; TWI = T-wave inversions.
In addition to these patterns, anterior TWI limited to leads V1 and V2 may be found in up to 14-28% of endurance athletes without an underlying disease process regardless of ethnicity, potentially due to physiologic right ventricular (RV) remodeling.6 Conversely, TWI not adhering to the patterns described earlier should be considered abnormal and the patient should undergo further testing. Lateral and/or inferolateral TWI are often associated with HCM and/or dilated cardiomyopathy, whereas abnormal anterior TWI may suggest arrhythmogenic right ventricular cardiomyopathy (ARVC); inferior TWI are less clearly correlated with a specific pathology but are not considered a normal physiologic response to training. Myocarditis and left ventricular noncompaction cardiomyopathy may also present with TWI. Some study data suggest that the presence of J-point elevation preceding anterior TWI indicates benign physiologic remodeling, whereas an isoelectric or depressed ST segment and extension of anterior TWI beyond lead V4 are more closely associated with ARVC and HCM7; however, these findings are not validated, and their presence or absence should not preclude further workup if indicated. Initial testing should consist of TTE, with a low threshold to obtaining cMRI if the TTE findings are nondiagnostic. Maximal exercise ECG testing and/or ambulatory ECG monitoring may be considered to evaluate for the presence of ventricular arrhythmias. Given the increased risk of sudden cardiac death in these pathologies, and because vigorous physical activity may accelerate the pathogenesis of certain conditions such as ARVC, restriction from exercise is reasonable pending results of initial workup.
This patient's ECG met one major criterion for ARVC: TWI in leads V1 through V3 in an individual >14 years of age without a complete right bundle branch block. Her history of RVOT-morphology PVCs is also concerning for ARVC-associated arrhythmia, particularly in the setting of her presentation with exertional dyspnea.
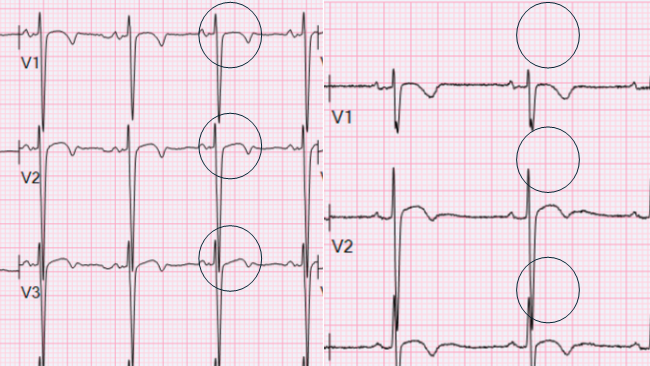
She underwent TTE and cMRI, which demonstrated severe RV enlargement and hypokinesis (Figure 4), meeting diagnostic criteria for ARVC.8 Electrophysiology study was performed given her history of PVCs, with findings revealing scarring along the anterior RVOT extending along the RV free wall, as well as multiform PVCs at rest that increased with isoproterenol infusion. After shared decision-making, she declined placement of an implantable cardiac defibrillator but agreed to undergo detraining and limit further vigorous physical activity. Repeat ECG and imaging after completion of detraining showed that her TWI had resolved, and her RV size and function returned to near-normal.
Figure 4: TTE and cMRI Demonstrating Severe RV Enlargement
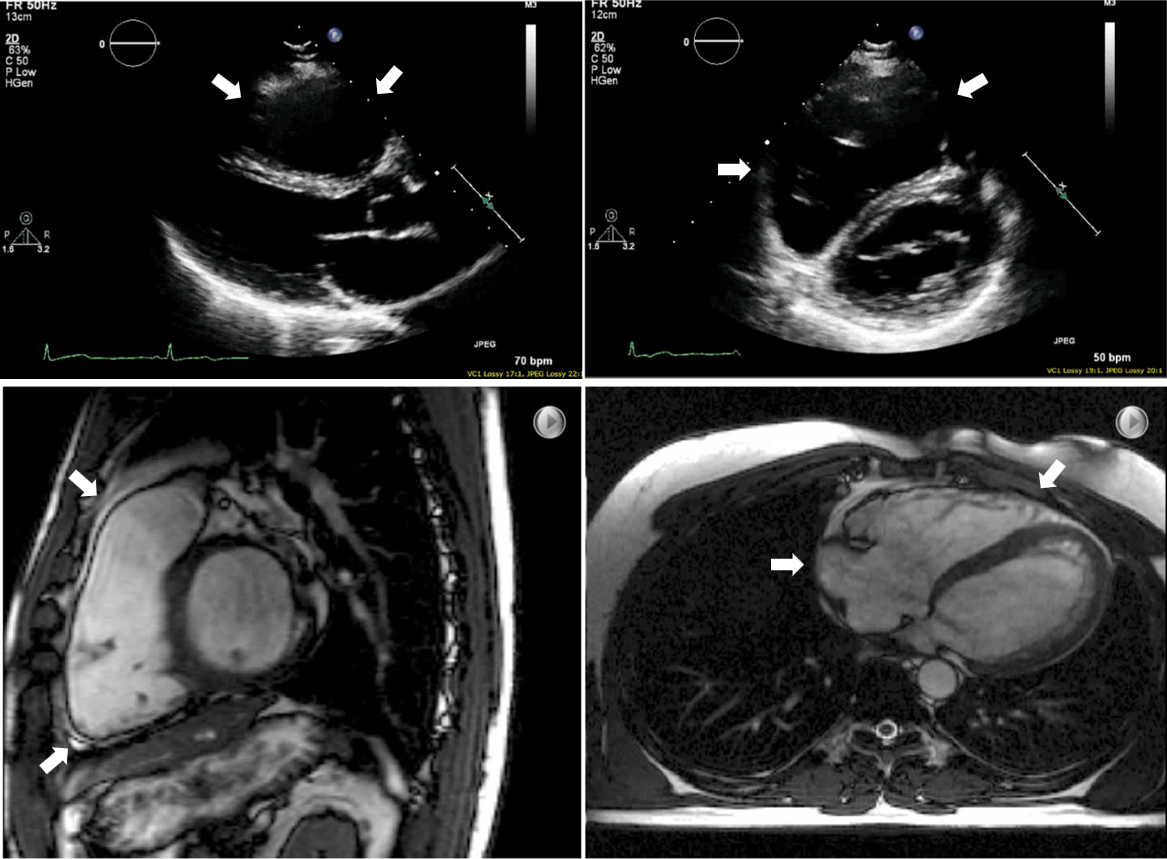
(Top panel). TTE. (Bottom panel) cMRI. Arrows show RV enlargement.
ECG = electrocardiogram; cMRI = cardiac magnetic resonance imaging; RV = right ventricle; TTE = transthoracic echocardiogram; TWI = T-wave inversions.
References
- Sharma S, Drezner JA, Baggish A, et al. International recommendations for electrocardiographic interpretation in athletes. J Am Coll Cardiol 2017;69:1057-75.
- D'Ascenzi F, Anselmi F, Berti B, et al. Prevalence and significance of T-wave inversion in children practicing sport: a prospective, 4-year follow-up study. Int J Cardiol 2019;279:100-4.
- Calore C, Zorzi A, Sheikh N, et al. Electrocardiographic anterior T-wave inversion in athletes of different ethnicities: differential diagnosis between athlete's heart and cardiomyopathy. Eur Heart J 2016;37:2515-27.
- Krishnan S, Guseh JS, Chukumerije M, et al.; American College of Cardiology Sports & Exercise Leadership Council. Racial disparities in sports cardiology: a review. JAMA Cardiol 2024;9:935-43.
- Papadakis M, Carre F, Kervio G, et al. The prevalence, distribution, and clinical outcomes of electrocardiographic repolarization patterns in male athletes of African/Afro-Caribbean origin. Eur Heart J 2011;32:2304-13.
- D'Ascenzi F, Anselmi F, Adami PE, Pelliccia A. Interpretation of T‐wave inversion in physiological and pathological conditions: current state and future perspectives. Clin Cardiol 2020;43:827-33.
- Zaidi A, Sheikh N, Jongman JK, et al. Clinical differentiation between physiological remodeling and arrhythmogenic right ventricular cardiomyopathy in athletes with marked electrocardiographic repolarization anomalies. J Am Coll Cardiol 2015;65:2702-11.
- Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J 2010;31:806-14.