A Stimulating Pediatric Electrocardiogram
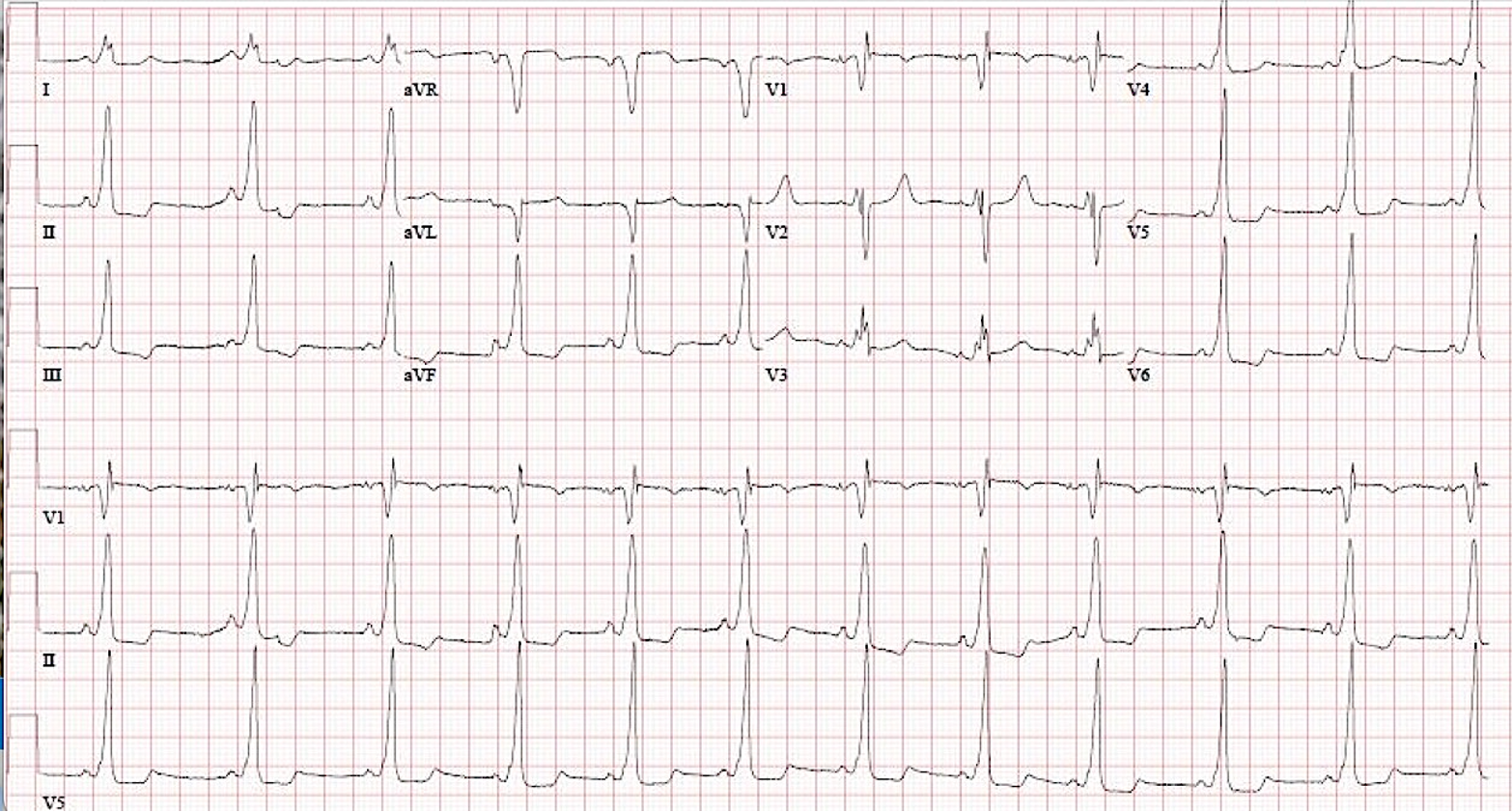
An electrocardiogram (ECG) is obtained in a 12-year-old boy before the initiation of stimulant medication to treat attention deficit hyperactivity disorder (Image 1). He has no cardiac symptoms. His family medical history is unremarkable, as are his cardiac physical examination and echocardiogram findings.
Image 1
Which one of the following would be the most appropriate next management step in most patients with a condition like this?
Show Answer
The correct answer is: D. Electrophysiology study.
This patient's ECG (Image 1) had findings of ventricular pre-excitation from an accessory pathway (AP) manifested as a delta wave and was consistent with Wolff-Parkinson-White (WPW) syndrome. Patients with WPW syndrome are at increased risk of the development of re-entrant supraventricular tachycardia. They are also at risk of sudden death from rapid anterograde conduction of atrial fibrillation (AF) over the AP causing ventricular fibrillation (VF), although this is rare. The incidence of sudden death is higher in young individuals.1 The risk of sudden death is present even among those without symptoms, and a life-threatening event may be the initial presentation of WPW syndrome.2,3 Data from a large claims dataset was used for evaluation of VF and life-threatening event risk (sudden death, aborted sudden death, or rapidly conducted AF) in an unselected pediatric population with WPW syndrome.4 A life-threatening event occurred in 49 patients (0.7%), including VF in 20 (0.3%). The incidence of VF was 0.8 events per 1,000 person-years, and the incidence of life-threatening events was 1.9 events per 1,000 person-years. There were no occurrences of VF in matched control patients. The rate of a life-threatening event was 70 times higher in patients with WPW syndrome (0.7%; 95% confidence interval [CI], 0.5-0.9%) than in control patients (0.01%; 95% CI, 0-0.02%).
All patients with pre-excitation—intermittent or persistent—regardless of symptom status are considered eligible for electrophysiology study (EPS) and possible ablation. Pediatric electrophysiologists demonstrate high willingness to move toward EPS in pathways, even for those deemed to be at low risk by noninvasive testing5; the new consensus guidelines are in line with this strategy.6
Recent data do not support sports restrictions in asymptomatic children with WPW syndrome. In a series of 96 children who experienced a life-threatening event, most events occurred during rest and routine activities of daily life.2
Initiating digoxin is an incorrect choice because this medication may not decrease the risks of arrhythmias or sudden death. There are EPS findings of digoxin possibly improving anterograde AP conduction in some patients with WPW syndrome.7
At present, most surveyed pediatric electrophysiologists do not trust noninvasive measures of anterograde refractoriness, such as exercise testing, to identify low-risk APs with high enough sensitivity to defer ablation.5 A study to evaluate the accuracy of exercise testing for predicting AP characteristics in children with WPW syndrome was conducted in 37 children who underwent exercise testing before an invasive EPS.8 The sudden loss of pre-excitation (i.e., disappearance of the delta wave) on exercise testing was seen in 10 patients (27%). However, no correlation was found between loss of pre-excitation and the anterograde AP effective refractory period or the shortest pre-excited R-R interval (SPERRI) in AF on EPS. Using SPERRI as the reference standard, the sensitivity for loss of pre-excitation was 24%, the specificity was 71%, the positive predictive value was 71%, and the negative predictive value was 24%. Thus, an exercise test was not accurate in detecting low-risk WPW syndrome.
References
- Obeyesekere MN, Leong-Sit P, Massel D, et al. Risk of arrhythmia and sudden death in patients with asymptomatic preexcitation: a meta-analysis. Circulation 2012;125:2308-15.
- Etheridge SP, Escudero CA, Blaufox AD, et al. Life-threatening event risk in children with Wolff-Parkinson-White syndrome: a multicenter international study. JACC Clin Electrophysiol 2018;4:433-44.
- Chubb H, Ceresnak SR. A proposed approach to the asymptomatic pediatric patient with Wolff-Parkinson-White pattern. Heart Rhythm Case Rep 2020;6:2-7.
- Janson CM, Millenson ME, Okunowo O, et al. Incidence of life-threatening events in children with Wolff-Parkinson-White syndrome: analysis of a large claims database. Heart Rhythm 2022;19:642-7.
- Chubb H, Campbell RM, Motonaga KS, Ceresnak SR, Dubin AM. Management of asymptomatic Wolff-Parkinson-White pattern by pediatric electrophysiologists. J Pediatr 2019;213:88-95.e1.
- Lampert R, Chung EH, Ackerman MJ, et al. 2024 HRS expert consensus statement on arrhythmias in the athlete: evaluation, treatment, and return to play. Heart Rhythm 2024;[ePub ahead of print].
- Sellers TD Jr, Bashore TM, Gallagher JJ. Digitalis in the pre-excitation syndrome. Analysis during atrial fibrillation. Circulation 1977;56:260-7.
- Dalili M, Vahidshahi K, Aarabi-Moghaddam MY, Rao JY, Brugada P. Exercise testing in children with Wolff-Parkinson-White syndrome: what is its value? Pediatr Cardiol 2014;35:1142-6.

