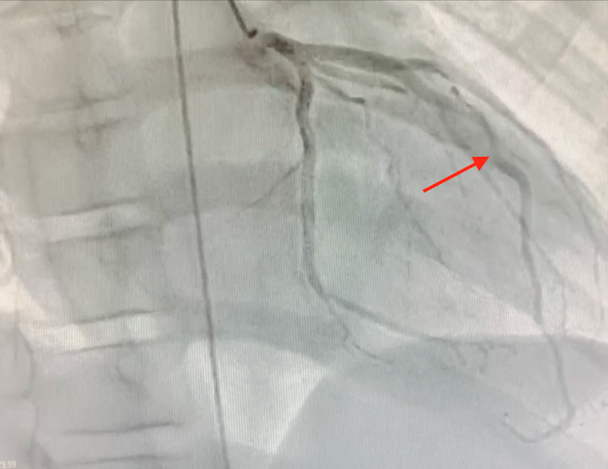
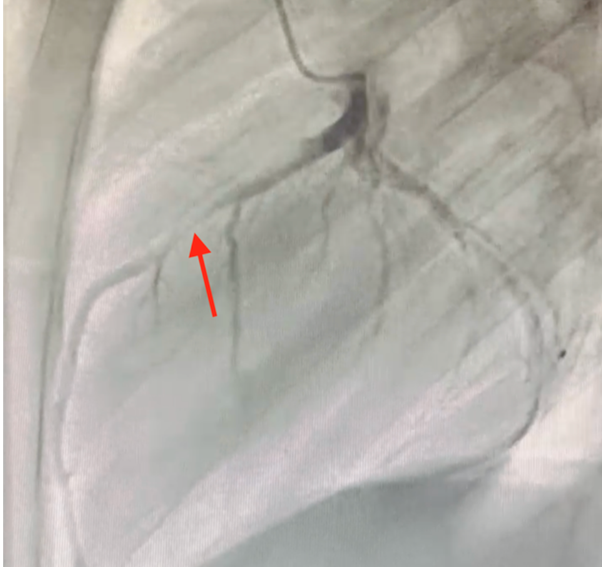
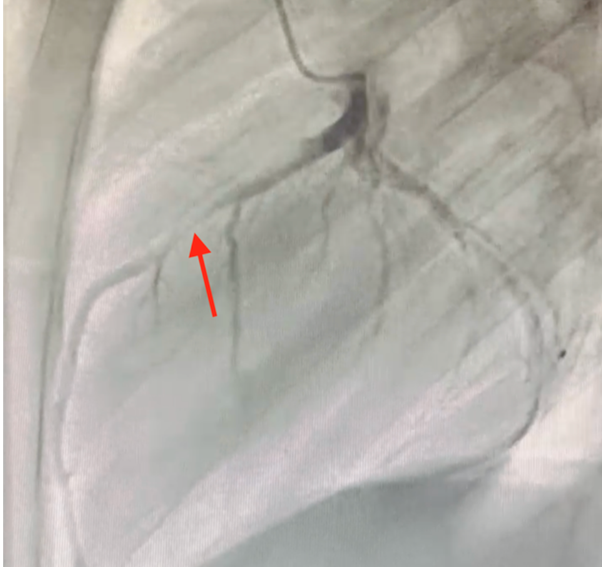
Myocardial bridge involving the LAD is the correct answer choice. This patient's angiograms demonstrated the typical finding of systolic narrowing of the midportion of the LAD (Images 1, 2 [arrows]) but normal appearance in diastole.1
Image 1: RAO 30-Degree Projection
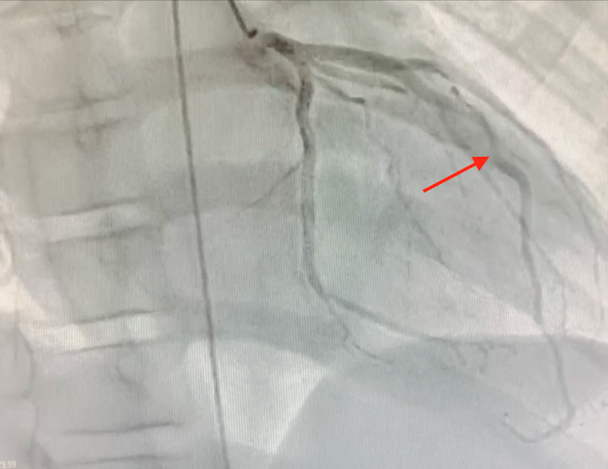 RAO = right anterior oblique.
RAO = right anterior oblique.
Image 2: Lateral Projection
There was no evidence of a coronary artery aneurysm, dissection, or anomalous connection to the coronary artery suggestive of a fistula.
Myocardial bridges have a prevalence of 15-85% reported by autopsy, 0.5-16% by coronary angiography, and 3.5-38.5% by computed tomography coronary angiography.1 Whereas most bridges are considered benign, specific anatomical characteristics (e.g., length, depth, and tortuosity), tissue properties (myocardial fiber orientation in relation to the coronary artery), and presence of hypertrophic cardiomyopathy influence the likelihood that they may cause symptoms or cardiac events.2 One must be careful in attributing symptoms to the presence of a myocardial bridge.3
Catheterization with coronary angiography, intravascular ultrasonography, and diastolic fractional flow reserve (dFFR) calculation may be helpful in assessing the clinical relevance and informing approaches to treatment.4 dFFR is defined as the ratio of mean coronary pressures measured directly distal and proximal to the stenosis obtained during cardiac catheterization. It is the index of choice for the assessment of functional severity of coronary artery stenosis. A value <0.75 during dobutamine stress represents clinically significant coronary compression due to a myocardial bridge.5
This patient's dFFR (0.89) suggested that the myocardial bridge was unlikely to cause coronary insufficiency and ischemia, and surgical unroofing was therefore not clearly indicated. The care team considered an invasive electrophysiology study to assess for inducible ventricular arrhythmias but, given his presentation, did not think it would add much to the treatment plan.6 Ultimately, shared decision-making with the family played a significant role in opting to not surgically unroof the myocardial bridge. He was diagnosed with idiopathic VF and an implantable cardioverter-defibrillator (ICD) was placed for secondary prevention of sudden cardiac death.7 Over the ensuing 12 months, he had two appropriate ICD shocks for VF while at rest and asleep at night, making the myocardial bridge a less likely culprit for his events. He is currently maintained on amiodarone therapy.
References
- Lee MS, Chen CH. Myocardial bridging: an up-to-date review. J Invasive Cardiol 2015;27:521-8.
- Roberts W, Charles SM, Ang C, et al. Myocardial bridges: a meta-analysis. Clin Anat 2021;34:685-709.
- Mohiddin SA, Begley D, Shih J, Fananapazir L. Myocardial bridging does not predict sudden death in children with hypertrophic cardiomyopathy but is associated with more severe cardiac disease. J Am Coll Cardiol 2000;36:2270-8.
- Ge J, Jeremias A, Rupp A, et al. New signs characteristic of myocardial bridging demonstrated by intracoronary ultrasound and Doppler. Eur Heart J 1999;20:1707-16.
- Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703-8.
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2018;72:e91-e220.
- Visser M, van der Heijden JF, Doevendans PA, Loh P, Wilde AA, Hassink RJ. Idiopathic ventricular fibrillation: the struggle for definition, diagnosis, and follow-up. Circ Arrhythm Electrophysiol 2016;9:[ePub ahead of print].