The correct answer is to start the mother on oral flecainide. The fetus had incessant tachycardia at a rate of 220 bpm, was preterm, and did not have hydrops. In this situation, the 2024 AHA scientific statement recommends transplacental flecainide as the first-line antiarrhythmic drug (AAD) of choice with frequent monitoring of fetal well-being and maternal drug toxicity.1
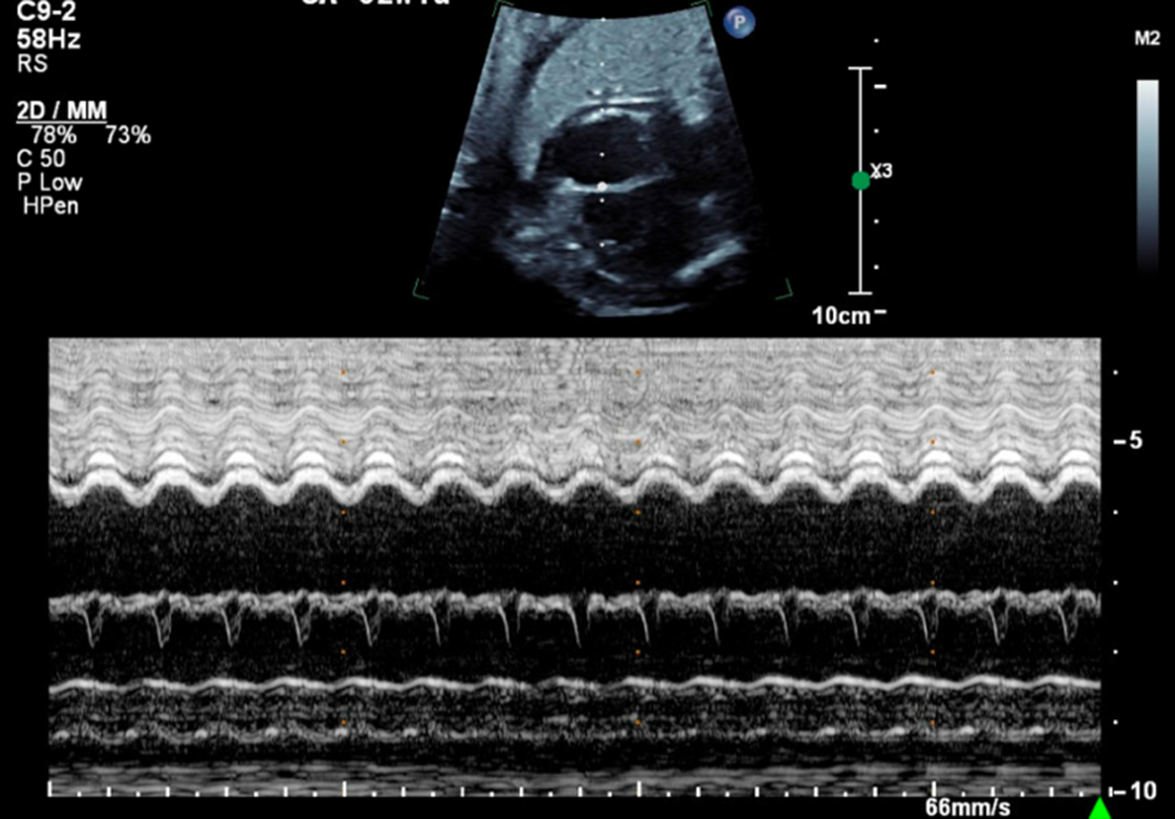
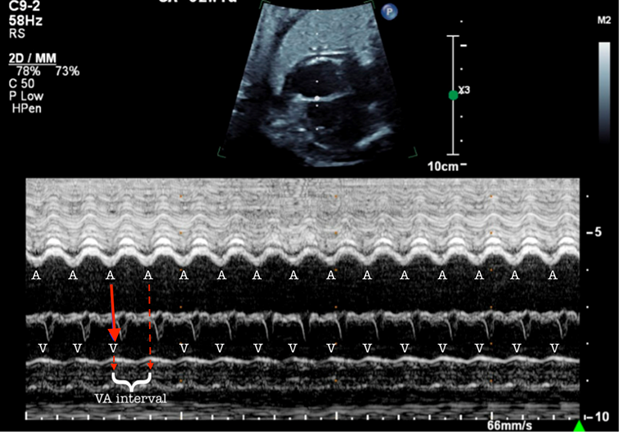
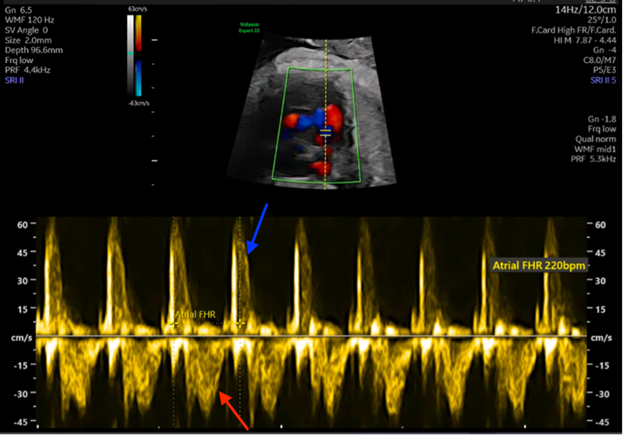
Figures 1 and 2 demonstrate a 1:1 atrial-ventricular (A-V) relationship, with one ventricular contraction for every atrial contraction and a short ventriculoatrial (VA) interval. Labeled versions of the images are shown in Figures 3 and 4. This fetus most likely had a re-entrant supraventricular tachycardia (SVT), which typically has a rate between 220 and 300 bpm and a 1:1 A-V relationship with a short VA interval (Figure 3). In contrast, ectopic atrial tachycardia, permanent junctional reciprocating tachycardia, and sinus tachycardia have a 1:1 A-V relationship with a long VA interval. In the setting of atrial flutter (AFL), atrial rates are typically 350-500 bpm with consistent or varying rates of atrioventricular (AV) block (2:1, 3:1, or 4:1). The resultant ventricular HRs are a proportional fraction of the atrial rate.
Figure 3: M‐Mode Tracing Through the RA and RV From a Four‐Chamber Image Demonstrates a 1:1 VA Relationship
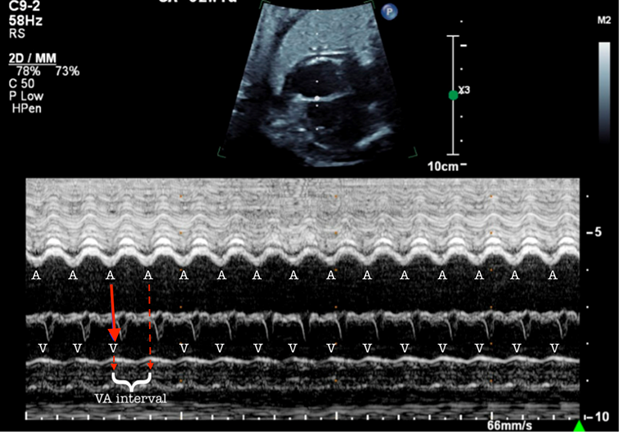 Figure 3: M‐Mode Tracing Through the RA and RV From a Four‐Chamber Image Demonstrates a 1:1 VA Relationship. Courtesy of Ramachandra R, Ho DY.
Figure 3: M‐Mode Tracing Through the RA and RV From a Four‐Chamber Image Demonstrates a 1:1 VA Relationship. Courtesy of Ramachandra R, Ho DY.
The interval between the V and A (the VA interval) is long.
A = atrial contraction; RA = right atrium; RV = right ventricle; V = ventricular contraction; VA = ventriculoatrial.
Figure 4: Simultaneous PW Doppler Interrogation of LV Inflow and Outflow Demonstrate a 1:1 A-V Relationship
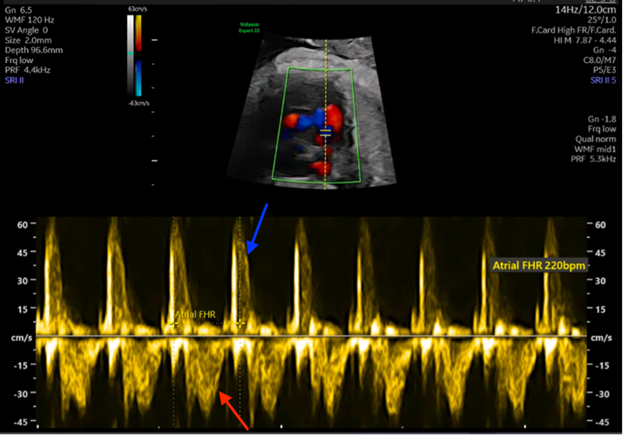 Figure 4: Simultaneous PW Doppler Interrogation of LV Inflow and Outflow Demonstrate a 1:1 A-V Relationship. Courtesy of Ramachandra R, Ho DY.
Figure 4: Simultaneous PW Doppler Interrogation of LV Inflow and Outflow Demonstrate a 1:1 A-V Relationship. Courtesy of Ramachandra R, Ho DY.
Red arrow: inflow wave from atrial contraction. Blue arrow: outflow wave from ventricular contraction.
A-V = atrial-ventricular; LV = left ventricular; PW = pulsed-wave.
This fetus was found to be in tachycardia for approximately 15 hours per day and thus met the criteria for incessant tachycardia, which is defined as tachycardia for >50% of the time or >12 hours per day. Otherwise, the diagnosis is an intermittent tachycardia.
For intermittent tachycardia, frequent monitoring for increased tachycardia burden and development of fetal hydrops is generally sufficient and poses fewer risks to the mother than does drug therapy. Fetuses with incessant tachycardia complicated by hydrops who are close to term should be delivered. Fetuses with incessant tachycardia with or without hydrops that, like this fetus (at 31 weeks' gestation), are not considered to be mature enough for delivery should be treated transplacentally (i.e., using oral medications taken by the mother) with flecainide. Frequent monitoring of fetal well-being and for maternal drug toxicity is also indicated.
There is an ongoing prospective multicenter trial to determine the best initial treatment for nonhydropic fetal SVT. On the basis of the current available evidence, the 2024 AHA scientific statement and 2023 HRS expert consensus statement suggest flecainide, if available, as the first-line AAD of choice to treat fetal SVT.1,2 The results of a meta-analysis demonstrated higher termination rates for AV re-entrant tachycardia with flecainide than with sotalol and digoxin.3 Flecainide was also found to be superior to digoxin, particularly in the setting of hydrops.4 For fetuses with AFL, data from some studies suggest a superior termination rate when treated with sotalol than with digoxin or flecainide.1 In immature fetuses with incessant SVT complicated by hydrops that do not respond to treatment with transplacental drug therapy alone, direct fetal intramuscular injection of digoxin can be added as the next step.5
References
- Batra AS, Silka MJ, Borquez A, et al.; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology, Council on Basic Cardiovascular Sciences, Council on Cardiovascular and Stroke Nursing, Council on Genomic and Precision Medicine, and Council on Lifelong Congenital Heart Disease and Heart Health in the Young. Pharmacological management of cardiac arrhythmias in the fetal and neonatal periods: a scientific statement from the American Heart Association. Circulation 2024;149:e937-e952.
- Joglar JA, Kapa S, Saarel EV, et al. 2023 HRS expert consensus statement on the management of arrhythmias during pregnancy. Heart Rhythm 2023;20:e175-e264.
- Hill GD, Kovach JR, Saudek DE, Singh AK, Wehrheim K, Frommelt MA. Transplacental treatment of fetal tachycardia: a systematic review and meta-analysis. Prenat Diagn 2017;37:1076-83.
- Alsaied T, Baskar S, Fares M, et al. First-line antiarrhythmic transplacental treatment for fetal tachyarrhythmia: a systematic review and meta-analysis. J Am Heart Assoc 2017;6:[ePub ahead of print].
- Parilla BV, Strasburger JF, Socol ML. Fetal supraventricular tachycardia complicated by hydrops fetalis: a role for direct fetal intramuscular therapy. Am J Perinatol 1996;13:483-6.