Sara is a 65-year-old woman with long-standing type 2 diabetes mellitus (DM), hypertension, hyperlipidemia, and hypothyroidism. She is morbidly obese and has chronic kidney disease (CKD) with a glomerular filtration rate (GFR) of 65 ml/min/m2. She complains of fatigue but has no chest pain. She is still able to do her activities of daily living, but has become less active, which she attributes to weight gain. She has not been able to walk upstairs for the last year and tends to walk slower than her family at the mall. She has occasional palpitations and wakes up during the night to go to the bathroom. She frequently wakes up with a headache and believes her increased fatigue is due to insomnia.
Physical Exam
- Blood pressure 146/ 89 mm Hg, pulse 93 bpm
- Body mass index 43 kg/m2, waist circumference 102 cm
- Exam: no murmur, short neck, jugular venous distention difficult to assess, S3
- Mild ankle edema of the left lower extremity, varicose veins, distal pulses palpable 2+
Medications
- Metformin 1000 mg BID and saxagliptin 50 mg
- Pioglitazone 30 mg
- Pitavastatin 4 mg and ezetimibe 10 mg (had leg cramps with atorvastatin and rosuvastatin)
- On amlodipine 10 mg/perindopril 10 mg
- Levothyroxine 75 µg daily
- Furosemide 40 mg daily was started recently by her primary care physician for the edema
Basic Investigations
- Hemoglobin Aa1c (Hb A1C) 7.4%
- Low-density lipoprotein cholesterol 72 mg/dl, triglycerides 210 mg/dl, non–high-density lipoprotein cholesterol (non–HDL-C) 121 mg/dl, apolipoprotein B 130 mg/dl
- High-sensitivity C-reactive protein 2.1 mg/L
- Thyroid-stimulating hormone 2.1 mIU/L
- Abnormal liver function test (LFT): aspartate aminotransferase 46 U/L and alanine aminotransferase 57 U/L; presumed diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatosis
- Serum creatinine 1.3 mg/dl, GFR 57 ml/min/1.73 m2, urine albumin-to-creatinine ratio 78 mg/g (CKD stage 3)
- Electrocardiogram (ECG): left atrial enlargement (LAE) with left ventricular hypertrophy (LVH)
Extended Investigations
- Referred for sleep apnea evaluation because of uncontrolled hypertension and her symptoms – during sleep study, noted to have both sinus bradycardia and episodes of rapid atrial fibrillation (AF) during apnea episodes
- Sleep study confirmed moderate to severe obstructive sleep apnea (OSA)
- Referred to cardiology due to the AF during sleep study
- N-terminal pro-B-type natriuretic peptide 932 (elevated)
- ECG repeated: normal sinus rhythm with LVH and LAE
- Echocardiogram: normal LV ejection fraction (LVEF) 55%, dilated LA (4.1 cm), grade 2 diastolic dysfunction
- Mild pulmonary hypertension with right ventricular systolic pressure of 42 mm Hg
- Cannot exercise: 2 minutes on Bruce protocol exercise stress test with hypertensive response and severe dyspnea
- Coronary computed tomography angiography: mild nonobstructive plaque in left anterior descending (LAD) (40-50% soft plaque in LAD with calcium score 138)
- Due to morbid obesity and OSA and elevated Hb A1c, the endocrinologist switched her from saxagliptin to glucagon-like peptide-1 receptor agonist (GLP-1 RA) once weekly subcutaneous injectable
- Icosapent ethyl capsules 2 g twice daily is added for management of residual risk with high triglycerides and non–HDL-C
- Started on continuous positive airway pressure for OSA
- Referred for consideration of bariatric surgery
The correct answer is: E. Both B and D.
Undiagnosed congestive HF (CHF) in the outpatient setting, especially HFpEF, is a very common clinical presentation in high-risk diabetic patients. An echo study in asymptomatic DM patients with ECG abnormalities showed that 64% had HFpEF confirmed with tissue Doppler imaging.
CHOICE E
Choice E is the best answer, as both choices B and D are appropriate.
CHOICE B
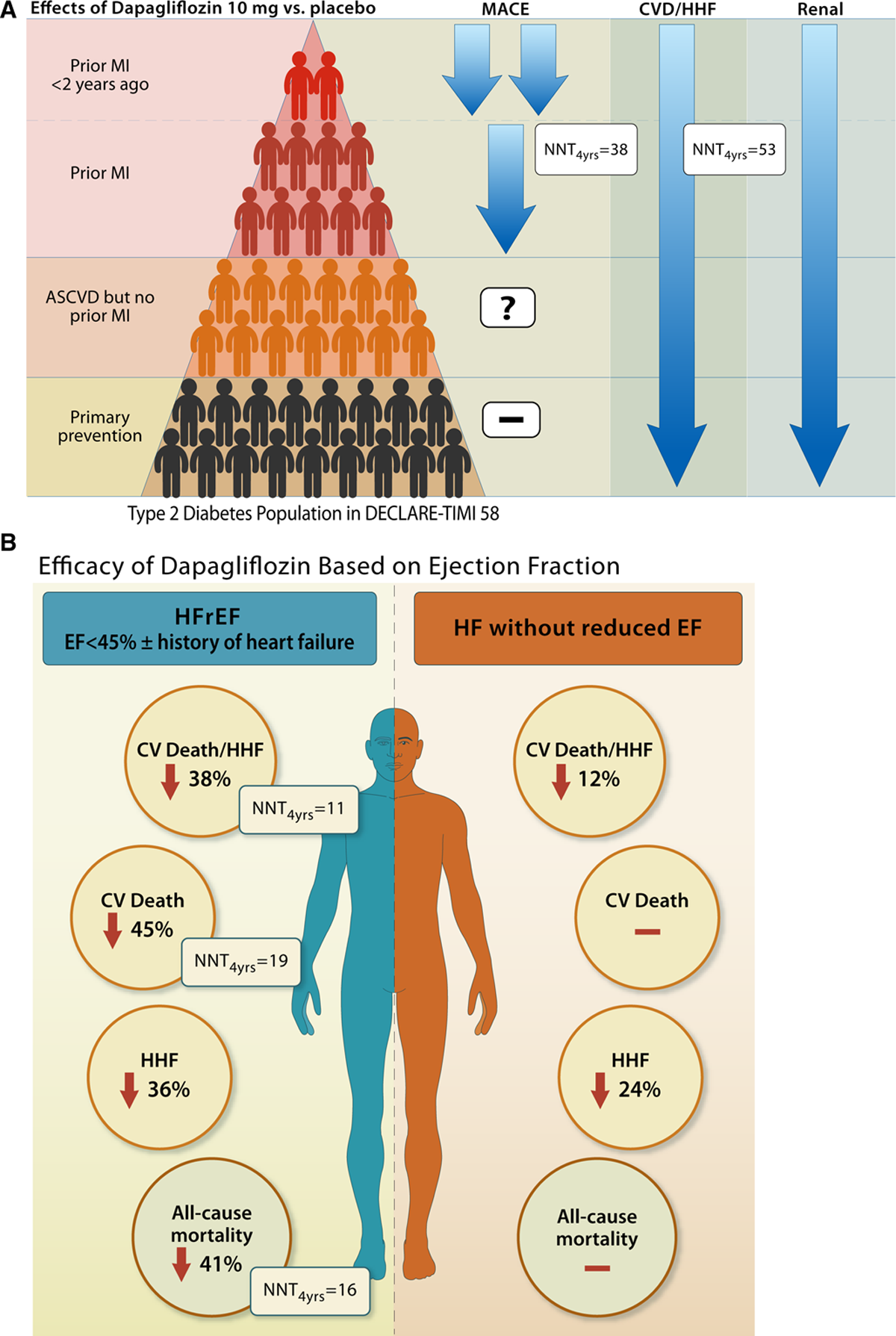
Choice B is correct. In DM patients with atherosclerotic CV disease or CKD with CHF, the American Diabetes Association and European Society of Cardiology guidelines broadly recommend either SGLT-1 or GLP-1 RA. The glucosuric effect of SGLT-2 inhibitors is well characterized and may result in volume depletion and hypotension if combined with diuretics; thus, reduction of the dose of diuretics is recommended. In all the trials – DECLARE–TIMI 58, EMPA-REG OUTCOME, and CANVAS – <10% of the patients had HF with reduced EF (HFrEF) with an EF of <40% and clinical CHF; nevertheless, a profound reduction of HF was observed across all three trials. Therefore, any diabetic patient with evidence of preserved, reduced, or mid-range HF would benefit from being on an SGLT-2 inhibitor and the lower the EF, the greater the benefit. Analysis of the DECLARE–TIMI 58 trial showed that dapagliflozin reduces hospitalized HF in a broad spectrum of patients with type 2 DM and high CV risk regardless of EF, with greatest absolute risk reduction in patients at highest risk, and reduces CV death and all-cause mortality in patients with HFrEF, especially EF <30%, as illustrated in Figure 1.
Figure 1
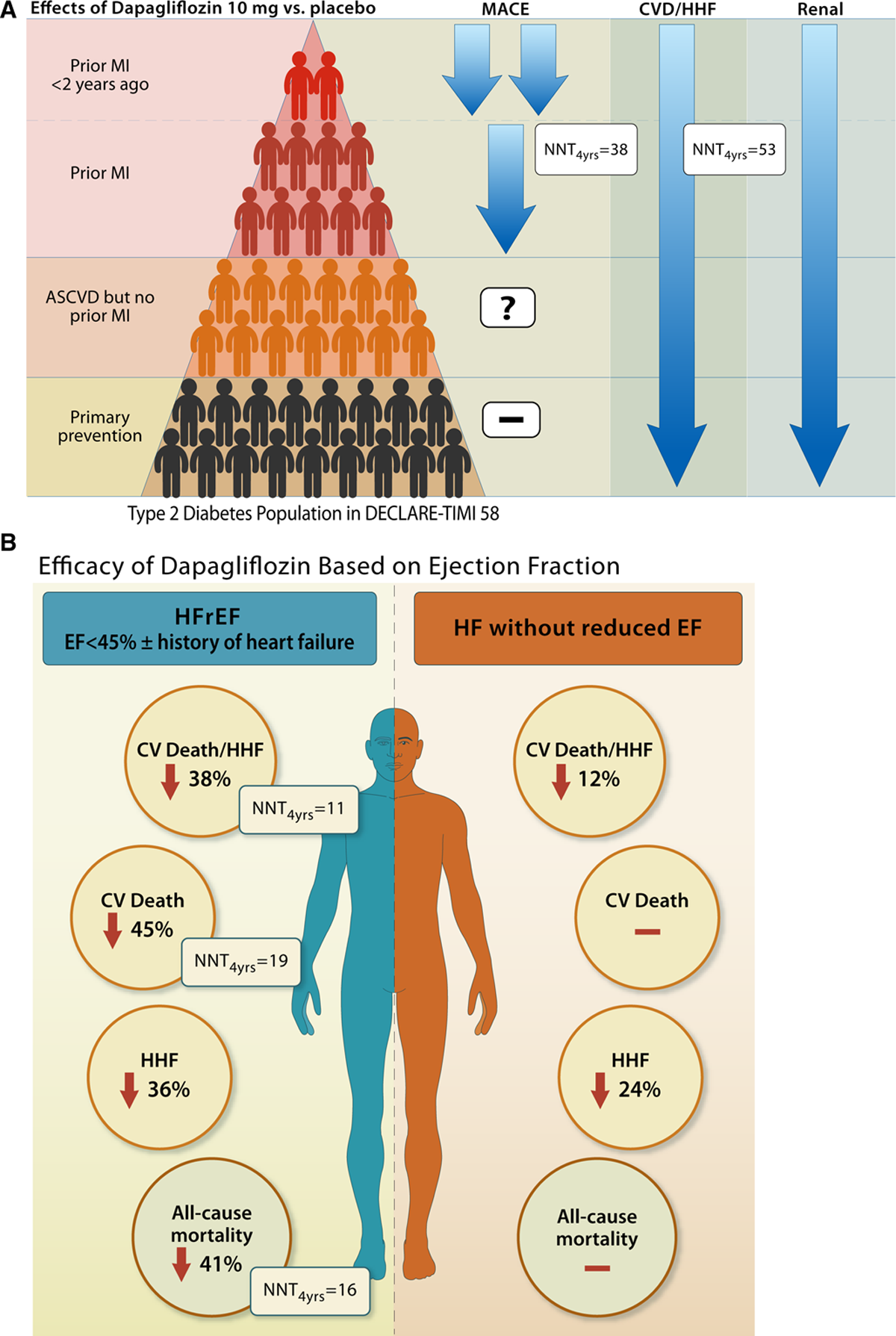 Reproduced with permission from Verma S, McMurray JJV. The serendipitous story of SGLT2 inhibitors in heart failure: new insights from DECLARE-TIMI 58. Circulation 2019;139:2537-41.
Reproduced with permission from Verma S, McMurray JJV. The serendipitous story of SGLT2 inhibitors in heart failure: new insights from DECLARE-TIMI 58. Circulation 2019;139:2537-41.
CHOICE D
Choice D is correct. The CHA2DS2-VASc score is 4 – female, hypertension, DM, CHF with GFR above 60 – TSOAC/DOAC at standard-dose dabigatran 150 mg BID, rivaroxaban 20 mg, or apixaban 5 mg BID are all appropriate.
CHOICE A
Choice A is incorrect. Pioglitazone is a thiazolidinedione (TZD) peroxisome proliferator-activated receptor (PPAR) gamma/insulin sensitizer and should be stopped completely because the patient has clinical CHF with lower extremity edema. The Food and Drug Administration has issued a black box warning regarding unmasking of CHF with TZDs. Pioglitazone in addition can increase LFTs and should not be continued if LFTs are 2.5x upper limit of normal.
CHOICE C
Choice C is incorrect. In this patient who is morbidly obese, weight loss is an important objective as is avoiding hypoglycemia. Adding sulfonylurea to achieve intensive glycemic control has been shown to increase weight gain and cause hypoglycemia with negative CV outcome. Saxagliptin has a black box warning in CHF and should be stopped. Conversely GLP-1 RA will improve weight loss (up to 11 kg) and CV outcomes. Hypoglycemia does not occur with GLP-1 RA or SGLt2-I except when combined with sulfonylurea and insulin. Hypoglycemia significantly worsens CV outcome in DM with CAD and CHF.
Due to morbid obesity, OSA, as well as elevated Hb A1c with a new diagnosis of CHF, in addition to starting SGLT-2 I she is appropriately switched from saxagliptin to a GLP-1 RA.
Educational grant support provided by: Boehringer Ingelheim Pharmaceuticals.
References
- American Diabetes Association. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl 1):S98-S110.
- Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur Heart J 2020;41:255-323.
- Davies MJ, D'Alessio DA, Fradkin J, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2018;61:2461-98.
- Furtado RHM, Bonaca MP, Raz I, et al. Dapagliflozin and cardiovascular outcomes in patients with type 2 diabetes and prior myocardial infarction: subanalysis from the DECLARE-TIMI 58 trial. Circulation 2019;139:2516-27.
- Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta‐analysis of cardiovascular outcome trials. Lancet 2019;393:31-9.
- Boyer JK, Thanigaraj S, Schechtman KB, Pérez JE. Prevalence of ventricular diastolic dysfunction in asymptomatic, normotensive patients with diabetes mellitus. Am J Cardiol 2004;93:870-5.
- Retnakaran R, Zinman B. Thiazolidinediones and clinical outcomes in type 2 diabetes. Lancet 2009;373:2088-90.
- Home PD, Pocock SJ, Beck-Nielsen H, et al. Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet 2009;373:2125-35.
- Patel A, MacMahon S, Chalmers J, et al., on behalf of the ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-72.
- Duckworth W, Abraira C, Moritz T, et al., on behalf of the VADT Investigators. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129-39.
- Zoungas S, Patel A, Chalmers J, et al., on behalf of the ADVANCE Collaborative Group. Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410-18.
- Lam CSP, Chandramouli C, Ahooja V, Verma S. SGLT‐2 inhibitors in heart failure: current management, unmet needs, and therapeutic prospects. JAHA 2019;8:e013389.
- Kato ET, Silverman MG, Mosenzon O, et al. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation 2019;139:2528-36.
- Verma S, McMurray JJV. The serendipitous story of SGLT2 inhibitors in heart failure: new insights from DECLARE-TIMI 58. Circulation 2019;139:2537-41.