State-of-the-Art Review Provides Strategies to Address Post-TAVR CDs and PPI
A State-of-the-Art review published in JACC: Cardiovascular Interventions covers the epidemiology, clinical implications, risk factors and preventive strategies for new-onset conduction disturbances (CDs) and the need for permanent pacemaker implantation (PPI) after TAVR, which the authors note are a limitation of this therapy.
Most studies reviewed by authors Jorge Nuche, MD, et al., place the median incidence of new-onset left bundle branch block (LBBB) around 20% and PPI >10% after TAVR, and they note that the lack of uniformity regarding the reporting of CDs contributes to the range of rates seen across the studies. Both LBBB and PPI are associated with an increased risk of mortality and rate of heart failure hospitalization. Other CDs in this setting can include first-, second-, or third-degree atrioventricular block and intraventricular conduction delay with QRS complex ≥120 ms.
Regarding predicting CDs in TAVR, the authors describe a number of nonmodifiable risk factors, including preexisting right bundle branch block (RBBB), strongly associated with PPI, and other CDs as well as anatomic features such as membranous septal (MS) length, tapered eccentric left ventricular outflow tract and presence of calcium. They discuss the pros and cons of strategies for managing patients with baseline RBBB, including a temporary pacemaker, pre-TAVR ambulatory continuous ECG (AECG), prophylactic PPI and a screw-in temporary lead.
Modifiable risk factors include procedural aspects such as valve type, implant depth, valve oversize, and balloon predilatation and postdilatation. They write that “Refined implantation techniques, aiming to reduce the interaction between the valve frame and the conduction system,” have shown promising results in reducing the rate of CDs and PPI. Changes in transcatheter heart valves by manufacturers have helped to facilitate a higher valve implant.
Strategies before, during and after TAVR to prevent CDs are reviewed and outlined in a figure for handy reference. Before TAVR, along with a risk assessment including consideration of AECG and an RBBB protocol, preprocedural planning includes correct sizing, assessing risk of coronary occlusion/sinus sequestration, MS length and tailored THV selection. During the procedure, aim for a higher implant, perhaps through cusp overlap or radiolucent line-guided implant, and minimize steps. After the procedure, a management protocol should be followed and right ventricular pacing reduced.
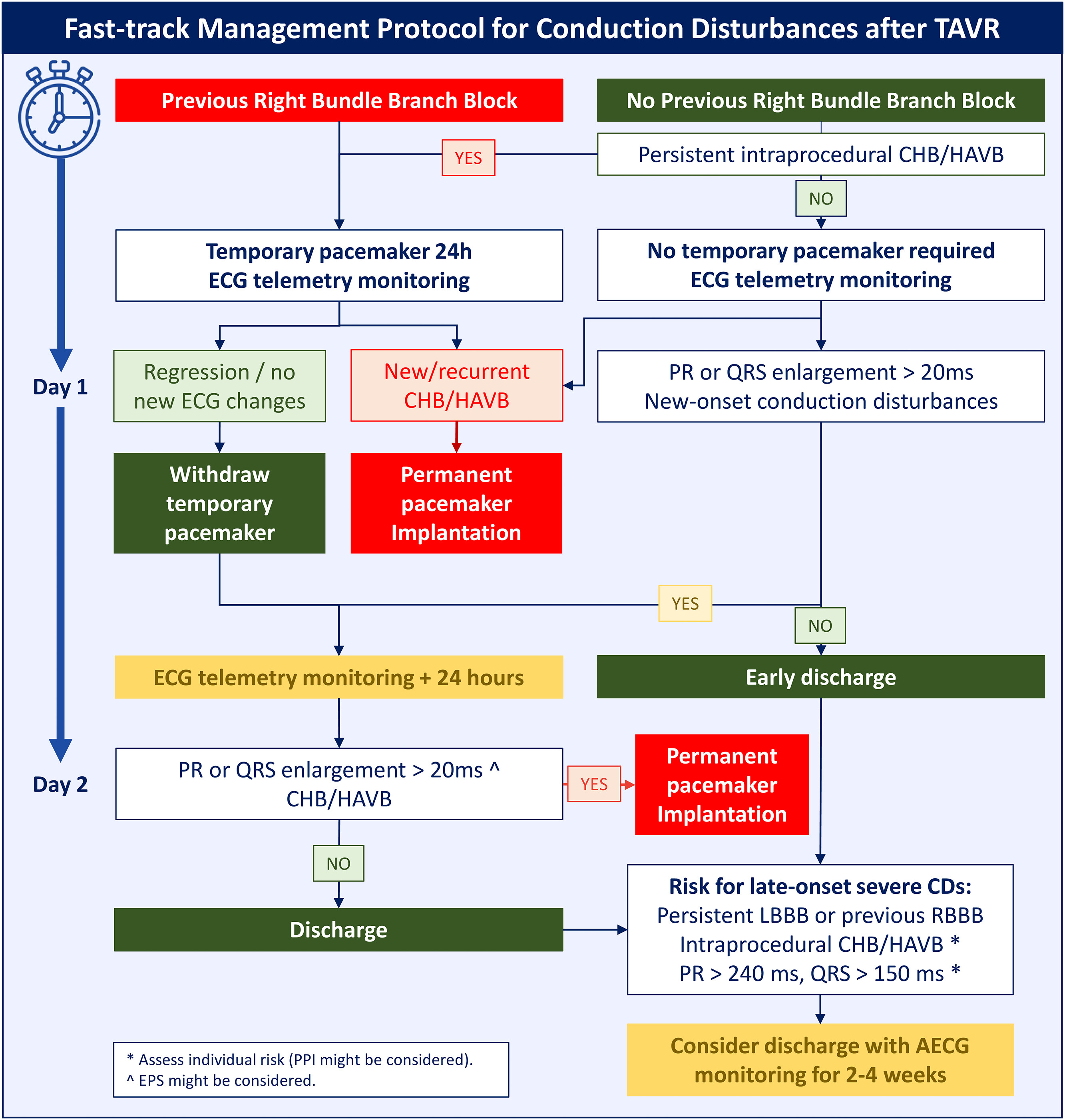
The authors propose a fast-track protocol for managing CDs after TAVR, aimed at reducing the length of stay and its related complications, with an algorithm for patients with and without RBBB at baseline. The protocol streamlines the decision-making process to a series of decision points over the first 48 hours post procedure and incorporates baseline RBBB, new or recurrent CDs, and ECG telemetry results. “Ambulatory monitoring systems could be a valuable tool for detecting late onset conduction disturbances in patients benefiting from an early discharge strategy,” they write.
The authors identify a number of areas of future study to minimize CDs in patients who undergo TAVR. Future studies are warranted to assess the feasibility and results of redo TAVR and the impact of high implantation depth. Results are awaited from a number of ongoing trials listed by the authors that are evaluating strategies for prevention, early detection and reduction of PPI-related post TAVR. Efforts are also underway to address patients who develop advanced CDs.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, EP Basic Science, Cardiac Surgery and Arrhythmias
Keywords: Bundle-Branch Block, Transcatheter Aortic Valve Replacement
