COVID-19 and Hypertension: What We Know and Don't Know
Introduction to COVID-19
Coronavirus disease 2019 (COVID-19) emerged in December 2019 likely as a result of zoonotic transmission from wild animals linked to a large wet market in Wuhan, China.1 The responsible virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1 is a novel coronavirus that belongs to the same family as severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV). Due to its high transmissibility, COVID-19 spread quickly and escalated into a global pandemic. As of June 18, 2020 there were over 8 million documented cases and 450,000 deaths worldwide, including more than 2 million cases and 118,000 deaths in the United States (US).2
Early reports from major COVID-19 epicenters including Wuhan and Lombardy, Italy revealed higher morbidity and mortality rates among patients with a history of hypertension, coronary artery disease, diabetes mellitus, chronic kidney disease, and obesity. Since SARS-CoV-2 infects human cells via the angiotensin-converting enzyme II (ACE2) receptor that acts on the renin-angiotensin-aldosterone system (RAAS), a key regular of blood pressure, questions have been raised about a possible link between hypertension and severe COVID-19 infection. This paper will explore the current state of our understanding of this association and review recently published studies evaluating outcomes of hypertensive COVID-19 patients treated with RAAS inhibitors.
Link between Hypertension and COVID-19
Hypertension, defined by the American College of Cardiology (ACC) and American Heart Association (AHA) as a systolic blood pressure (BP) ≥130 or diastolic BP ≥80 mm3, is a primary modifiable risk factor associated with atherosclerotic cardiovascular disease.3 The prevalence of hypertension in US adults is around 50% and higher rates correlate directly with advancing age.3 According to the Centers for Disease Control (CDC), 63% of adults over the age of 60 are hypertensive,4 a number that will continue to rise as our population ages. Approximately 50% of US patients with hypertension are prescribed angiotensin converting enzyme inhibitors (ACE-I), aldosterone receptor blockers (ARB) and aldosterone antagonists, collectively called RAAS inhibitors, and are among the most frequently prescribed anti-hypertensive medications.5
Initial reports from COVID-19 hot spots, including Wuhan,6,7 Lombardy,8,9 and New York City,10 identified higher rates of hypertension among severely ill, hospitalized COVID-19 patients. A large US study of 5,700 hospitalized patients revealed an overall hypertension rate of 56%,10 similar to hypertension rates reported from China11 and Italy9 (50% and 49%, respectively). Despite these observations, the link between hypertension and COVID-19 is unclear. Severity of COVID-19 illness is skewed towards the elderly population who have a higher prevalence of hypertension. The median age of hospitalized patients in Lombardy and New York City was 63 years old9,10 and the percentage with a hypertension diagnosis is consistent with the percentage observed in the general population. While there is an overrepresentation of hypertension among hospitalized and critically ill COVID-19 patients, it is uncertain whether this relationship is causal or confounded by age and other co-morbidities associated with hypertension including obesity, diabetes mellitus, and chronic kidney disease.
SARS-CoV-2 and Interaction with the Renin-Angiotensin Aldosterone System
ACE2 is a modulator of the RAAS, a critical neurohormonal pathway that regulates blood pressure and fluid balance.12 The end product of the RAAS, angiotensin II, is a key vasoactive hormone that binds to angiotensin II receptor type 1 (AT1) located in the heart, lungs, blood vessels, kidneys, and adrenal glands, and it plays a central role in myocardial hypertrophy and fibrosis, inflammation, vascular remodeling, and atherosclerosis.13 ACE2 is expressed in many human tissues including the nasal epithelium, heart, kidneys, and lungs, and inactivates angiotensin II diminishing its vasoconstrictive and myoproliferative effects.14
SARS-CoV-2 binds to the ACE2 receptor via its spike (S) protein to allow entry into host cells. This complex is endocytosed leading to down-regulation of ACE2 and resulting in local accumulation of angiotensin II. Severe respiratory illness is a hallmark of COVID-19 and a primary cause of morbidity- and mortality-local activation of the RAAS is proposed as a mechanism for severe lung injury.14
Impact of RAAS Inhibitors on COVID-19 Patient Outcomes
Given the overrepresentation of hypertension among critically ill COVID-19 patients, concerns have been raised about the potential risk associated with RAAS inhibitors. Recent discussions have debated whether ACE-Is and ARBs upregulate ACE2 expression thereby facilitating COVID-19 infection or contributing to more severe infection.15 Findings from animal studies have revealed inconsistent effects of RAAS inhibitors on ACE2 levels and tissue activity with some showing upregulation of ACE2,16 while others demonstrating no change.17 While there is a paucity of human data, in cross-sectional studies of patients exposed to long term RAAS inhibitor therapies, plasma ACE2 activity was not higher in treated subjects.18,19
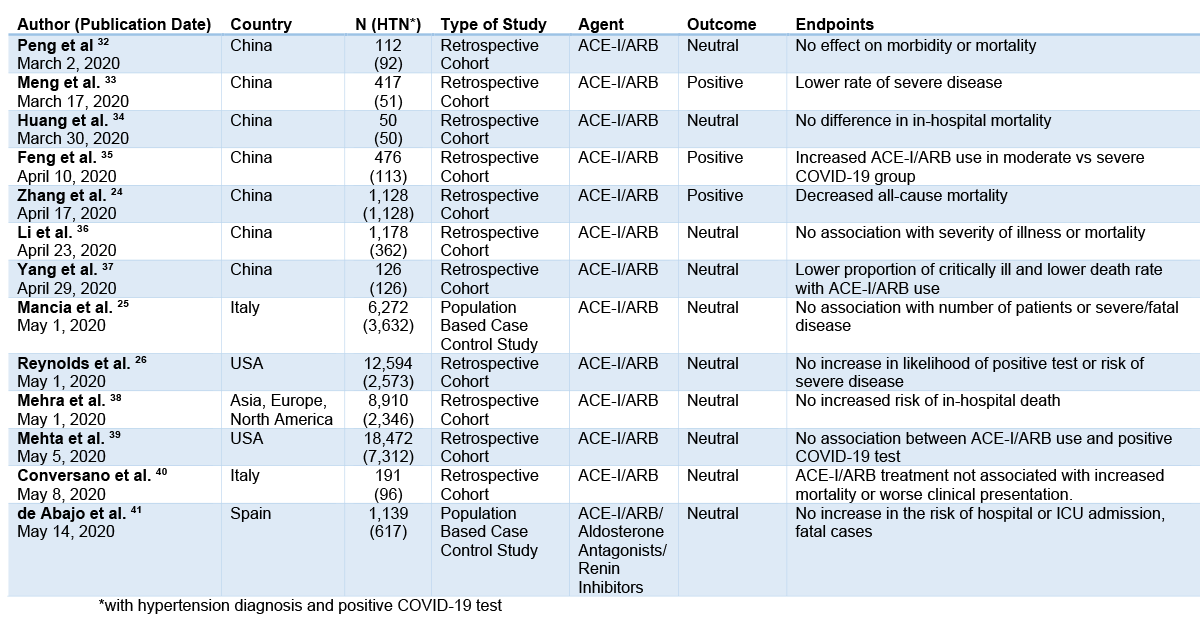
Due to concerns about the theoretical risk of RAAS inhibition in COVID-19 patients, some clinicians have recommended discontinuation of these antihypertensive agents. Currently, there is no compelling evidence that withdrawal of ACE-Is or ARBs prevents infection or impacts clinical outcomes.20,21 Many cases of myocardial infarction, myocarditis22 and cardiomyopathy23 have been reported among COVID-19 patients and interruption of cardioprotective medications, including RAAS inhibitors, could lead to clinical decompensation.14 A retrospective Chinese study of 1,128 hospitalized, hypertensive patients found that inpatient use of ACE-Is or ARBs was associated with a lower risk of all-cause mortality when compared to non-users.24 A recent case control data of 6,272 patients from Lombardy considered disease severity based on ACE-I or ARB use. This study demonstrated that neither ARBs nor ACE-Is had a significant association with COVID-19 cases or fatal outcomes.25 Reynolds et al. reported no interaction between any antihypertensive medication classes, including RAAS inhibitors, and risk of COVID-19 infection.26 Most of the peer-reviewed studies published to date have not found higher rates of infection, greater severity of disease, or increased mortality among patients with treated with RAAS inhibitors (Table 1). Of note, no studies have addressed the safety of initiating RAAS inhibitor therapy for disease-specific indications such as congestive heart failure. Recent statements by major medical societies have only commented on continuation or cessation of RAAS inhibitors for guideline-directed indications but have not provided guidance on initiation of therapy in COVID-19 patients.27
Table 1: RAAS Inhibitors and COVID-19 Patient Outcomes
Conclusion
The COVID-19 pandemic has taken an enormous toll on human life and efforts to better understand how to prevent and reduce severity of the disease are paramount. While overrepresentation of hypertension has been observed among critically ill COVID-19 patients, our current knowledge is skewed by observational studies that demonstrate an association but do not establish causation. The ACC, AHA, and Heart Failure Society of America released a joint statement advising against discontinuation of RAAS inhibitors where clinically indicated.27 This position is also supported by major international scientific societies including the International Society of Hypertension, European Society of Hypertension, European Society of Cardiology, Canadian Cardiovascular Society, and Canadian Heart Failure Society.28 The ACC recently created a COVID-19 Hub29 to provide clinical COVID-19 guidance to the cardiovascular team and includes information on RAAS inhibitors30 for hypertension management.31
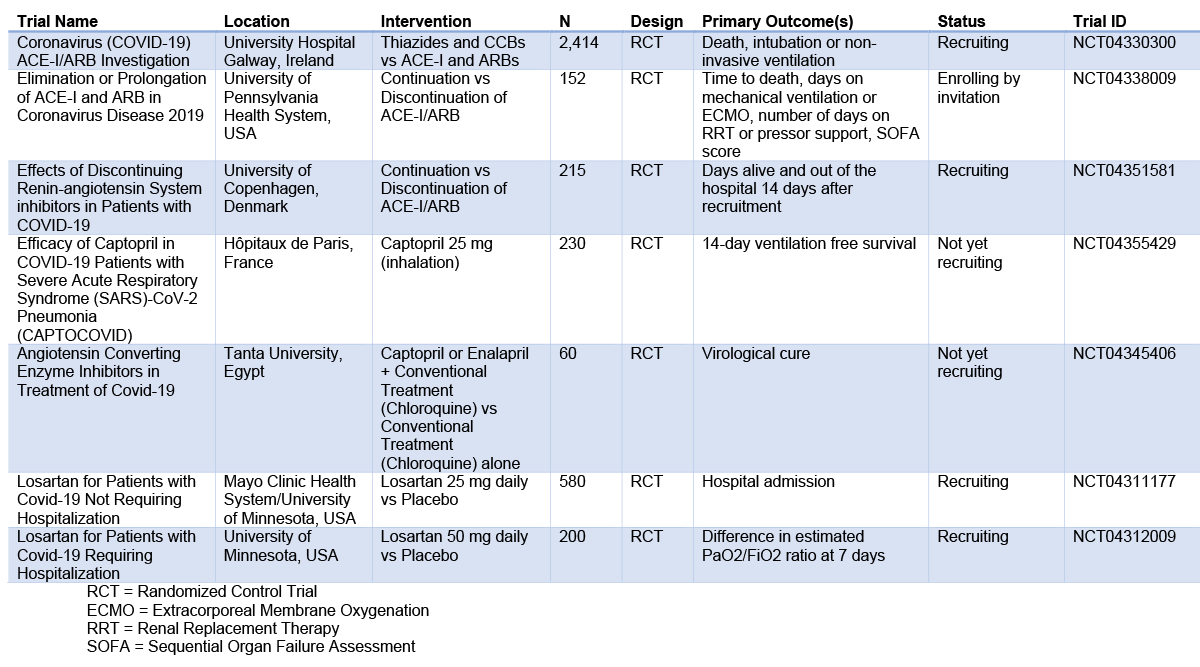
Studies are underway to explore whether hypertension is an independent risk factor for COVID-19. Given the theoretical risks of RAAS inhibition, randomized trials have been initiated to evaluate clinical outcomes for COVID-19 patients treated with ACE-Is or ARBs (Table 2). Until more information is available, it is important to treat hypertensive patients to target based on current clinical practice guidelines.
Table 2: Current Clinical Trials- Use of RAAS Inhibitors and COVID-19 Outcomes
References
- Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 2020;20:363-74.
- COVID-19 Dashboard by the Center for Systems Science and engineering (CSSE) at Johns Hopkins (Johns Hopkins University & Medicine website). 2020. Available at: https://coronavirus.jhu.edu/map.html. Accessed 04/30/2020.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol 2019;74:e177–232.
- Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief 2017;289:1–8.
- Shah SJ, Stafford RS. Current trends of hypertension treatment in the United States. Am J Hypertens 2017;30:1008–14.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13.
- Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020 March [Epub ahead of print].
- Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020 April [Epub ahead of print].
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020 April 22 [Epub ahead of print].
- Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical characteristics of patients who died of coronavirus disease 2019 in China. JAMA Netw Open 2020;3:e205619.
- Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA 2020 May [Epub ahead of print].
- Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344–56.
- Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med 2020;382:1653–9.
- Patel AB, Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA 2020 March [Epub ahead of print].
- Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension 2004;43:970–6.
- Burchill LJ, Velkoska E, Dean RG, Griggs K, Patel SK, Burrell LM. Combination renin-angiotensin system blockade and angiotensin-converting enzyme 2 in experimental myocardial infarction: implications for future therapeutic directions. Clin Sci (Lond) 2012;123:649–58.
- Walters TE, Kalman JM, Patel SK, Mearns M, Velkoska E, Burrell LM. Angiotensin converting enzyme 2 activity and human atrial fibrillation: increased plasma angiotensin converting enzyme 2 activity is associated with atrial fibrillation and more advanced left atrial structural remodelling. Europace 2017;19:1280–7.
- Epelman S, Shrestha K, Troughton RW, et al. Soluble angiotensin-converting enzyme 2 in human heart failure: relation with myocardial function and clinical outcomes. J Card Fail 2009;15:565–71.
- Messerli FH, Siontis GCM, Rexhaj E. COVID-19 and renin angiotensin blockers: current evidence and recommendations. Circulation 2020;141:2042-4.
- Brojakowska A, Narula J, Shimony R, Bander J. Clinical implications of SARS-Cov2 interaction with renin angiotensin system. J Am Coll Cardiol 2020;75:3085-95.
- Zeng J-H, Liu Y-X, Yuan J, et al. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection 2020 April [Epub ahead of print].
- Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020;323:1612-14.
- Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020;126:1671-81.
- Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin–angiotensin–aldosterone system lockers and the risk of Covid-19. N Engl J Med 2020;382:2431-40.
- Reynolds HR, Adhikari S, Pulgarin C, et al. Renin–angiotensin–aldosterone system inhibitors and risk of Covid-19. N Engl J Med 2020;382:2441-8.
- Bozkurt B, Kovacs R, Harrington B. HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19 (ACC.org website). 2020. Available at: https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. Accessed 05/01/2020.
- Iaccarino G, Borghi C, Cicero AFG, et al. Renin-angiotensin system inhibition in cardiovascular patients at the time of COVID19: much ado for nothing? A statement of activity from the Directors of the Board and the Scientific Directors of the Italian Society of Hypertension. High Blood Press Cardiovasc Prev 2020;27:105–8.
- American College of Cardiology COVID Hub (ACC.org website). 2020. Available at: https://www.acc.org/latest-in-cardiology/features/accs-coronavirus-disease-2019-covid-19-hub. Accessed 05/22/2020.
- Yang E, Kanwal A, Agarwala A, Martin L, Handberg E. What is the role of RAAS inhibitors in COVID-19? (ACC.org website). 2020. Available at: https://www.acc.org/latest-in-cardiology/articles/2020/04/29/12/42/key-questions-faq-on-covid-19-coronavirus-disease-2019-and-cardiovascular-disease#three. Accessed 05/22/2020.
- Yang E, Agarwala A, Martin L, Kanwal A, Handberg E. What is the link between hypertension and COVID-19? (ACC.org website). 2020. Available at: https://www.acc.org/latest-in-cardiology/articles/2020/04/29/12/42/key-questions-faq-on-covid-19-coronavirus-disease-2019-and-cardiovascular-disease#twelve. Accessed 05/22/2020.
- Peng YD, Meng K, Guan HQ, et al. [Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV]. Zhonghua Xin Xue Guan Bing Za Zhi 2020;48:E004.
- Meng J, Xiao G, Zhang J, et al. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect 2020;9:757–60.
- Huang Z, Cao J, Yao Y, et al. The effect of RAS blockers on the clinical characteristics of COVID-19 patients with hypertension. Ann Transl Med 2020;8:430.
- Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multi-center study of clinical features. Am J Respir Crit Care Med 2020;201:1380-8.
- Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol 2020;109:531–8.
- Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91–5.
- Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med 2020;382:e102.
- Mehta N, Kalra A, Nowacki AS, et al. Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020 May [Epub ahead of print].
- Conversano A, Melillo F, Napolano A, et al. RAAs inhibitors and outcome in patients with SARS-CoV-2 pneumonia. A case series study. Hypertension 2020 May [Epub ahead of print].
- de Abajo FJ, Rodríguez-Martín S, Lerma V, et al. Use of renin–angiotensin–aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet 2020 May [Epub ahead of print].
Clinical Topics: COVID-19 Hub, Heart Failure and Cardiomyopathies, Prevention
Keywords: Primary Prevention, Secondary Prevention, COVID-19, Pandemics, Coronavirus, Coronavirus Infections, severe acute respiratory syndrome coronavirus 2, Antihypertensive Agents, SARS Virus, Mineralocorticoid Receptor Antagonists, Blood Pressure, Renin-Angiotensin System, Angiotensin-Converting Enzyme Inhibitors, Aldosterone, Peptidyl-Dipeptidase A, Angiotensin II, Receptors, Mineralocorticoid
< Back to Listings